Neonatal Quality Improvement 2
Session: Neonatal Quality Improvement 2
079 - Taming The Temps: A Quality Improvement Initiative to Improve Newborn Admission Temperatures
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 79.6766
Chiamaka Aneji, McGovern Medical School, Houston, TX, United States; Rebekah L. Wilkinson, Children's Memorial Hermann Hospital, Houston, TX, United States; Maura Ryan, Childrens memorial hermann, Houston, TX, United States; Emma Sanchez, Children's Memorial Hermann Hospital, Houston, TX, United States; Holly Tonry, Childrens Memorial Hermann, houston, TX, United States; Bettina Hebert, UTHealth McGovern School of Medicine, Houston, TX, United States; Amir M. Khan, McGovern Medical School at the University of Texas Health Science Center at Houston, Houston, TX, United States; Olivia Russell, McGovern Medical School at the University of Texas Health Science Center at Houstony, Houston, TX, United States; Catherine Wong, University of Texas Health Science Center Houston, Webster, TX, United States; Aman Jain, McGovern Medical School at the University of Texas Health Science Center at Houston, Houston, TX, United States; Valerie Wood, Children's Memorial Hermann Hospital, Kingwood, TX, United States; Carly Shahbazian, Children's Memorial Hermann Hospital, Houston, TX, United States; Krysten Webber, Children’s Memorial Hermann Hospital, Spring, TX, United States
.jpg)
Chiamaka Aneji, MBBS, MPH
Associate Professor of Pediatrics
McGovern Medical School
Houston, Texas, United States
Presenting Author(s)
Background: Maintaining normal temperature is a critical function for newborn survival. Abnormal body temperature (ABT) following birth is an important global problem affecting newborns of all gestational ages (GA) and birth weights (BW). The recommended neonatal body temperature range is 36.5 C - 37.5 C. Newborn ABT is associated with increased risk of morbidity and mortality. A wet newborn can lose up to 4C in the first twenty minutes of life, a critical time period when delivery room (DR) newborn resuscitation is typically done. ABT remains a significant problem in newborns admitted from the DR to the neonatal intensive care unit (NICU) despite targeted interventions in the past 6 years. In the past 12 months 27% of all newborns admitted to the NICU had abnormal temperatures.
Objective: Achieve 40% reduction in the rate of ABT on NICU admission from the baseline of 27 % by 18 months in all newborns inborn in delivery areas of the hospital and directly admitted to the NICU after birth by standardizing DR processes.
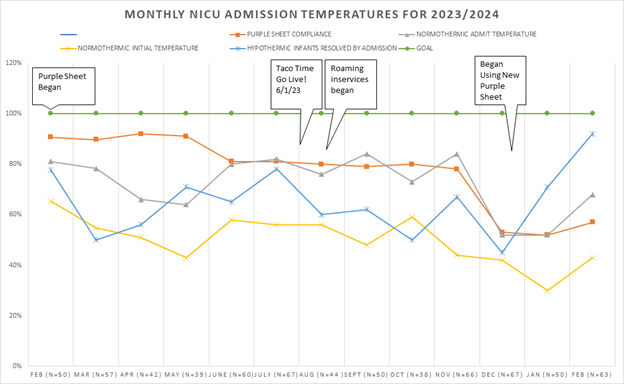
Design/Methods: The quality improvement (QI) methodology was used to develop this initiative. Pre-intervention efforts focused on stakeholder buy-in and education. Three Plan-Do-Study-Act (PDSA) cycles were implemented. The ‘Temperature Journey’ process of measuring newborn temperatures at designated times in the DR along with the 'Purple Sheet', a DR data collection tool for documenting and tracking the measured newborn temperatures, were developed and implemented in January 2023. ‘TACO TIME’, a thermoregulation process for ≤ 34 6/7 weeks GA and/or ≤ 2500g estimated fetal weight was implemented in June 2023. The ‘Ride Tag - Must be 36.5 C to ride’, a standardized approach for DR ABT corrective steps was implemented February 2024.
Primary outcome: first measured temperature on NICU arrival from DR.
Balancing measure: admission temperature > 37.5C.
Results: We achieved a mean reduction in ABT of 41% (range 15 - 52%). Normothermia improved from 71% in 2022 to 76% and 85% respectively in 2023 and 2024. There was > 90% reduction in mild hypothermia. The greatest improvement was in preterm newborns BW < 1500 grams. The average newborn admission temperature was 36.7 C. There was no increase in hyperthermia (temperature > 37.5C) above baseline.
Conclusion(s): The QI initiative achieved decreased rates of newborn ABT on NICU admission after implementing 3 PDSA cycles. The project transitioned to maintenance phase in August 2024 and efforts have been developed around sustainability. Future directions involve scaling up by implementation of this successful initiative at all the DRs across the hospital system.
Figure 1: Root causes of newborn abnormal admission temperatures
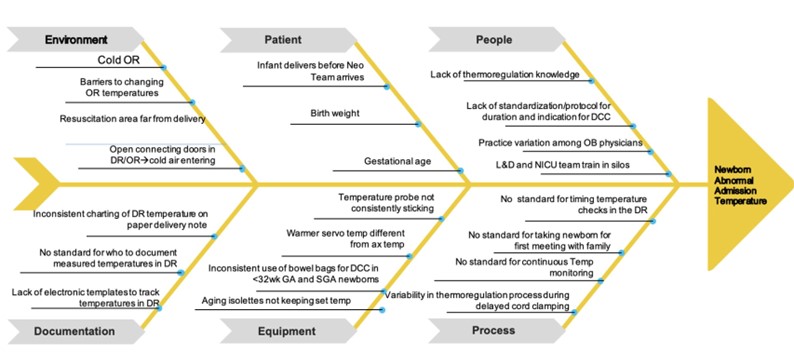
Figure 2: Admission temperature < 36 C by birth weight
.jpg)
Figure 3: Monthly NICU admission temperature rates