Neonatal Quality Improvement 2
Session: Neonatal Quality Improvement 2
080 - The Cub Club: A Quality Improvement Initiative to Increase Euthermia and Timely Administration of Surfactant and Dextrose in Extremely Preterm Infants
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 80.6745
Shoshana Newman-Lindsay, University of California Davis Children's Hospital, Sacramento, CA, United States; Paulina Hume, University of California Davis Children's Hospital, 612 El Dorado Way, CA, United States; Christa Bedford-Mu, UC Davis, Sacramento, CA, United States; Alina Harper, University of California Davis Children's Hospital, Elk Grove, CA, United States; Katy Wright, University of California Davis Children's Hospital, Sacramento, CA, United States; Emily Stieren, University of California Davis Children's Hospital, Sacramento, CA, United States
- PH
Paulina Hume, MD
Fellow
University of California Davis Children's Hospital
612 El Dorado Way, California, United States
Presenting Author(s)
Background: Extremely preterm infants are highly vulnerable to both short- and long-term complications. Though survival has improved, rates of neurodevelopmental impairment remain high. The period immediately following birth is particularly vulnerable, and maintenance of euthermia and timely administration of dextrose, and if intubated, surfactant, are linked to improved outcomes.
Objective: UC Davis Children’s Hospital has been developing a small baby program, the “Cub Club,” for inborn infants < 27 weeks or < 1000g. The ultimate goal of the “Cub Club” is to improve survival and neurodevelopmental outcomes in this population, and admission processes were chosen as the first area of intensive focus and iterative improvements.
Design/Methods: Our aim was to increase the proportion of infants who remained euthermic and received surfactant and dextrose within the first 90 minutes of life to more than 50% within 1 year. This aim was limited to infants intubated in the delivery room in order to better standardize the process.
An interdisciplinary team was formed including physicians, nurse and NNP leaders, respiratory therapists, and a dietician. We identified and trained a team of bedside nurses to be “cub nurses,” and revised and disseminated the admission protocol. Cub nurses generated change ideas to improve thermoregulation in a structured brainstorming session (Fig 1).
Process measures were lowest temperature in the first six hours of life, time to dextrose (as fluids or starter TPN), and time to surfactant. Balance measure included hyperthermia (highest temperature in first 6h if >38.0).
Results: With iterative changes to admission processes in context of a small baby team, we improved euthermia in the first six hours of life, and reduced time to both dextrose fluids and surfactant (Table 1). As we began to reduce hypothermia, we saw an increase in hyperthermia without resolution of hypothermia, which we addressed by implementing change ideas generated by cub nurses (Fig 2). The shift in timely surfactant and dextrose most closely matched the timing of implementing our admission guidelines, and the shift in thermoregulation followed implementing ideas suggested by cub-trained nurses (Fig 2).
Conclusion(s): Interdisciplinary quality improvement initiatives can improve outcomes for ELBW infants. We intend this project to be the first phase in our effort to reduce severe IVH. Many efforts to improve thermoregulation focus on reducing admission hypothermia—the 6h time period and success in reducing hyperthermia set this project apart.
Figure 1: Key Driver Diagram for Euthermia
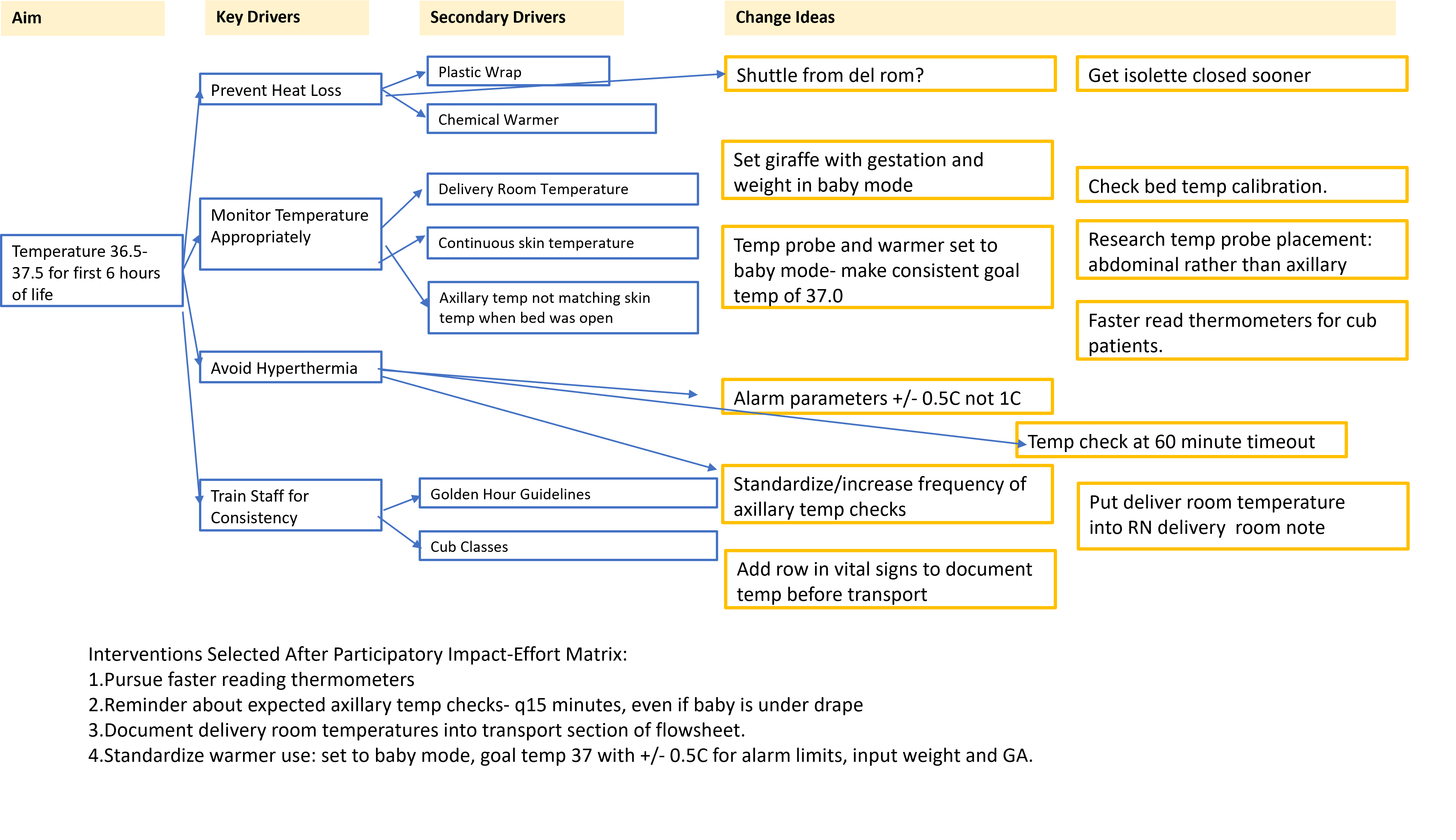 Introducing admission guidelines and specific RN training did not produce the sustained improvement in admission normothermia we were hoping for. To address this, a structured brainstorming session was held with the cub-trained nurses. We presented the framework of a key driver diagram (blue boxes) and added RN suggestions in the yellow boxes. These change ideas were then ranked on an impact-effort matrix and the high-impact low effort ideas noted on the bottom of the figure were introduced.
Introducing admission guidelines and specific RN training did not produce the sustained improvement in admission normothermia we were hoping for. To address this, a structured brainstorming session was held with the cub-trained nurses. We presented the framework of a key driver diagram (blue boxes) and added RN suggestions in the yellow boxes. These change ideas were then ranked on an impact-effort matrix and the high-impact low effort ideas noted on the bottom of the figure were introduced. Table 1: Summary of Demographics and Outcomes Data
.png) These groups are split by before and after the admission guidelines as we saw a change in the admission process then (Fig 2). *Statistically significant difference via t-test, p=0.004. **Statistically significant difference in pre- and post- groups via chi-square, p=0.009.
These groups are split by before and after the admission guidelines as we saw a change in the admission process then (Fig 2). *Statistically significant difference via t-test, p=0.004. **Statistically significant difference in pre- and post- groups via chi-square, p=0.009. Figure 2: Run and Control Charts
.png) Run chart for lowest temperature in first 6h of life (top), with the episodes of hyperthermia noted as orange dots on the date of admission. We noted new hyperthermia when we began planning this project. The grey line represents the baseline median of 36.4 C. Significant shifts are demarcated with green boxes. Below is a control chart showing minutes from birth to both dextrose-containing IV fluid and surfactant among infants intubated in the delivery room. The baseline group (11/2022-07/2023) averaged 135 minutes, which improved to 87 minutes. This shift occurred after implementation of our admission guidelines.
Run chart for lowest temperature in first 6h of life (top), with the episodes of hyperthermia noted as orange dots on the date of admission. We noted new hyperthermia when we began planning this project. The grey line represents the baseline median of 36.4 C. Significant shifts are demarcated with green boxes. Below is a control chart showing minutes from birth to both dextrose-containing IV fluid and surfactant among infants intubated in the delivery room. The baseline group (11/2022-07/2023) averaged 135 minutes, which improved to 87 minutes. This shift occurred after implementation of our admission guidelines.

