Emergency Medicine 8
Session: Emergency Medicine 8
121 - Using Video to Teach a Simplified Mass Casualty Triage System in a Pediatric Trauma Center
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 121.7086
George M. Smith, Riley Hospital for Children at Indiana University Health, Fishers, IN, United States; Roxanna Lefort, Indiana University School of Medicine, Carmel, IN, United States; Benton Hunter, Indiana University School of Medicine, Indianapolis, IN, United States; Kara Kowalczyk, Indiana University School of Medicine, Indianapolis, IN, United States
- GS
George M. Smith, Jr., MD (he/him/his)
Fellow- Pediatric Emergency Medicine
Riley Hospital for Children at Indiana University Health
Fishers, Indiana, United States
Presenting Author(s)
Background: Pediatric Mass Casualty Incidents (MCIs) are a thankfully rare occurrence. Maintaining Emergency Department (ED) readiness for such high risk, low frequency events presents a unique challenge. There are several MCI triage models used around the world, including some that have Pediatric-specific algorithms. However, all existing models are designed for healthcare systems and providers who do not primarily care for children. Given the existing comfort and competence of Pediatric EDs, a unit-specific MCI plan is potentially more efficient than existing universal models.
Objective: To determine the effectiveness of a Pediatric ED-specific training video distributed to ED physicians, non-physician providers, nurses, paramedics, and techs in a quaternary pediatric trauma center.
Design/Methods: A questionnaire was administered to evaluate participants' confidence in responding to an MCI within the pediatric ED using a Likert type scale. A test was also administered, asking participants to correctly sort 12 short clinical cases into the appropriate triage areas during an MCI. The video training modules instructed trainees on how to properly triage patients into one of 3 pathways within the Pediatric ED during an MCI. The video curriculum was provided to the staff of the Riley Hospital Pediatric ED. Both the questionnaire and quiz were then repeated after completion of the training module. Results were analyzed using paired t-test for the quiz and Mann Whitney U-test for the Likert scale survey.
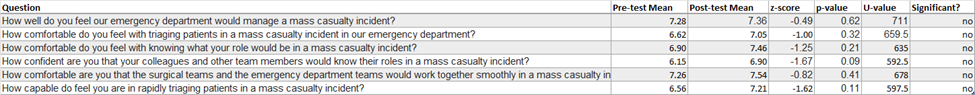
Results: 260 team members received the email invitation, the video was viewed 68 times, 63 total responses were submitted, and 40 (15%) completed both the pre- and post-training sections. For the quiz, the average pre- and post-intervention scores were 8.7 (SD 1.9) and 9.2 (SD 1.9) respectively, out of 12 This improvement was not statistically significant (p = 0.14). Similarly, there was no statistically significant change in confidence for any of the 6 survey questions after the intervention. (Table 1).
Conclusion(s): Our pediatric ED-specific training video did not result in a significant increase in knowledge or confidence among healthcare workers in a pediatric referral center. However, there were small improvements, and our study may have been underpowered. Limitations of the study include a small sample size, low overall response rate, and a robust existing multimodal MCI training already in place within the department. Video training modules may present a resource-efficient training modality that departments can use to train for low-frequency events, but more research is needed.
Table 1