Quality Improvement/Patient Safety 3
Session: Quality Improvement/Patient Safety 3
040 - Utilizing Neonatal Pain and Sedation score (N-PASS) as an objective tool for weaning and escalating sedative medications in neonatal patients.
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 40.7046
Jermine Harriet Romald, Childrens mercy, Overland Park, KS, United States; Jotishna Sharma, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Amy L. Marks, Children's Mercy Hospital, Kansas City, MO, United States; Alexandra Oschman, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States

Jermine Harriet Romald, MD, FAAP (she/her/hers)
Neonatology fellow
Childrens mercy
Overland Park, Kansas, United States
Presenting Author(s)
Background: Our NICU has utilized the Neonatal Pain and Sedation Scale (N-PASS) to assess and manage pain for over a decade. In August 2023 the unit implemented utilization of the sedation scoring portion of the N-Pass to objectively assess sedation and thereby wean or escalate sedation medications based on sedation targets. The process that was implemented included nursing assessment and charting of N-PASS scores on all neonates and infants who are on continuous infusion or scheduled sedative medications (defined as dexmedetomidine, lorazepam, midazolam, or morphine) in the NICU with every hands-on assessment. In addition, physicians are required to discuss sedation score target ranges during rounds and document the target sedation score in the daily progress note. At baseline, the N-PASS score for sedation is being charted by nursing staff 50% of the time. Neonatologists are documenting in their progress notes a daily target sedation score 25% of the time.
Objective: 1.Increase compliance of nursing assessment and documentation of N-PASS scores from 50% to 70% on all patients receiving continuous or scheduled sedatives by March 15th, 2024.
2.Increase compliance of physician documentation of N-PASS sedation score targets in daily progress notes from 25% to more than 50% by March 15th, 2024.
Design/Methods: Root cause of the problem was identified using a fish bone diagram. Primary drivers were lack of knowledge of the policy, lack of constant reminders or tasks, and difficulty finding charted scores in Cerner. Interventions that were made included: Didactic education session in Jan 2024 to entire ICN staff, weekly email reminders and modification for progress note templates to include prompts for target sedation scores and automatic drop in of sedation scores charted by nursing.
Results: Within a month of intervention, N-PASS sedation score charting by nurses increased to 74% from 50%. Target sedation scores were documented in progress notes 37% of the time compared to less than 25% prior to intervention. During our 2nd PDSA cycle we were able to further increase nursing charting to 80% and Physician documenting sedation target scores to 50%.
Conclusion(s): Simple methods like didactics and constant reminders go a long way in improving compliance of new policies and guidelines. Next steps are to improve utilization of the charted N-PASS scores and targets on weaning or escalating sedative medication doses. To do this, the next PDSA cycle will focus on addressing barriers to applying the scores to weaning and escalating of sedative medication doses.
Fish Bone Diagram
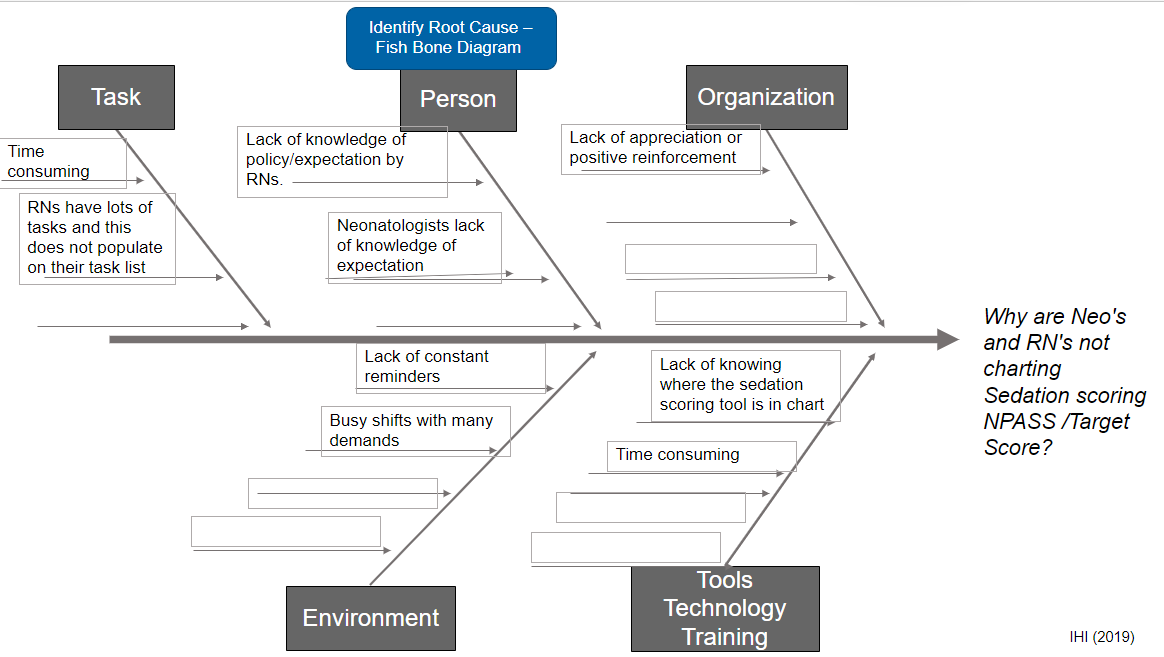 Identify Root Cause
Identify Root Cause Driver Diagram
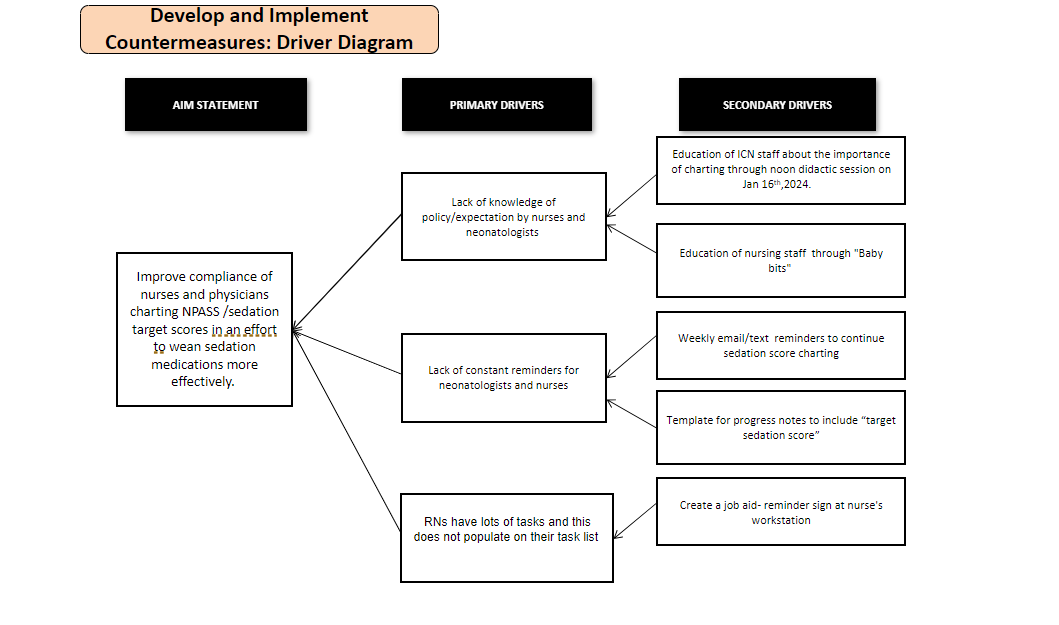 Develop and Implement Counter measures
Develop and Implement Counter measuresRUN Chart
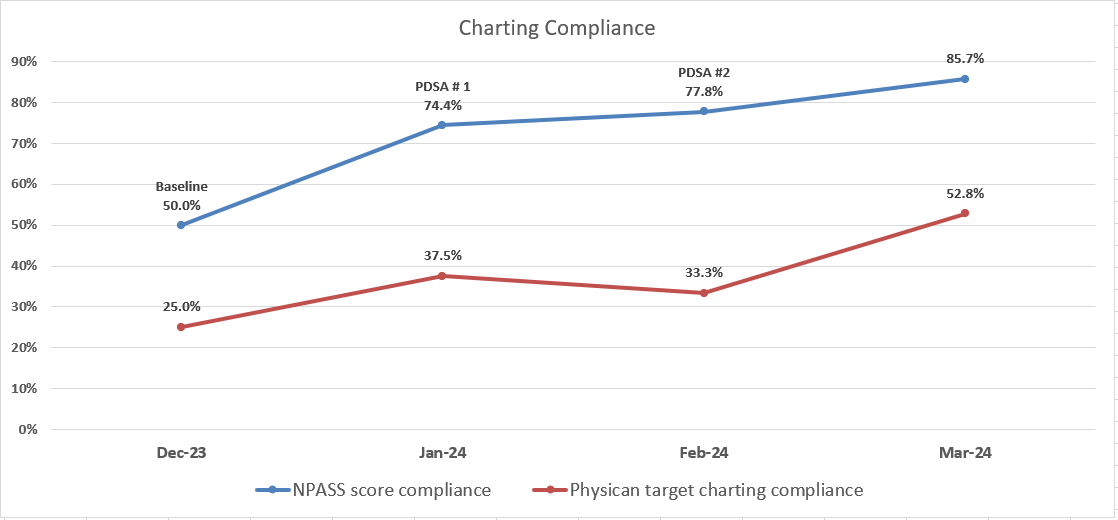 Charting Compliance
Charting Compliance

