Emergency Medicine 2
Session: Emergency Medicine 2
430 - Pediatric Readiness and Experience Caring for Children During Disaster and Surge Scenarios: A Mixed-methods Study of Rural and Critical Access Hospital Staff
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 430.6155
Anne Runkle, Ohio State University College of Medicine, Columbus, OH, United States; Michelle Moegling, UH Rainbow Babies & Children's Hospital, Cleveland, OH, United States; Erica Popovsky, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Leonardo Barrera, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Anna Bowie, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Anne Lakes, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Steven E. Krug, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States

Anne Runkle, MD (she/her/hers)
Assistant Professor of Pediatrics and Emergency Medicine
Ohio State University College of Medicine
Columbus, Ohio, United States
Presenting Author(s)
Background: Over 80% of pediatric emergency department (ED) visits are in community hospitals, which vary widely in their size and pediatric readiness. Rural and Critical Access Hospitals (CAHs) see few children and are challenged to remain proficient in caring for pediatric patients for both everyday care and in disaster scenarios.
Objective: To engage directly with healthcare providers in rural and CAH EDs to identify existing strengths and perceived needs and to uncover barriers to pediatric preparedness and disaster readiness.
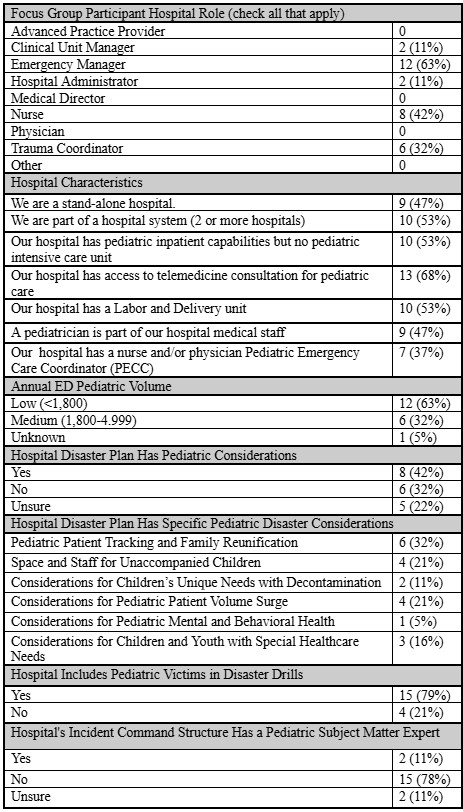
Design/Methods: We surveyed rural and CAH clinicians about their hospital’s pediatric care, including questions on patient volumes, inpatient capabilities, pediatric education, pediatric disaster considerations, and perceived gaps in available pediatric emergency resources. We solicited volunteers from survey respondents for focus groups. Semi–structured focus groups were conducted with 19 participants across five sessions from February-March 2024. Participants were identified and recruited from CAHs in the Health Resources and Services Administration Region 5 group (IL, IN, MI, MN, OH, WI). Deidentified focus group transcripts were analyzed using mixed-methods analysis software. A constant comparative approach was used to identify themes.
Results: We received 41 survey responses from clinicians including emergency nurses, emergency managers, trauma coordinators, and clinical unit managers. Most worked at low pediatric volume hospitals ( < 1800 annual pediatric patients), over half were part of a hospital system, and nearly half had capacity to admit some pediatric patients. Most did not have a Pediatric Emergency Care Coordinator or a pediatric disaster plan. Their most requested resources included education on respiratory emergencies, pediatric trauma, and sample pediatric protocols and policies. The 19 focus group participants had similar demographics to the survey respondents. Focus group analysis generated several themes: clinical strengths of staff at rural and CAHs, community involvement in pediatric education, desire for pediatric education resources specifically for rural and CAH, staffing limitations as a barrier to pediatric education, and desire for guidance on developing pediatric disaster plans.
Conclusion(s): Prior efforts to assess and promote pediatric readiness have demonstrated significant challenges in low volume hospitals. Our study engaged directly with clinicians at these institutions to explore facilitators and barriers to pediatric readiness and disaster preparedness. These results will be used to develop pediatric resources specifically for rural and CAH clinicians.
Table 1: Survey Participant Demographics and Selected Responses
.jpg)
Table 2: Focus Group Participant Demographics and Selected Responses
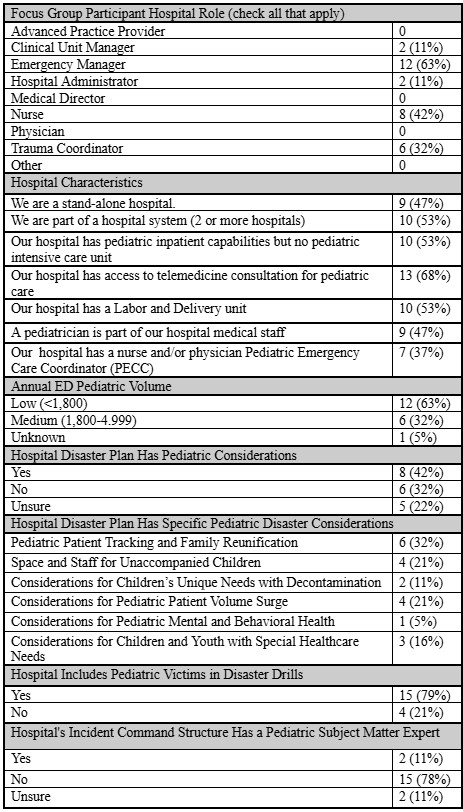
Table 1: Survey Participant Demographics and Selected Responses
.jpg)
Table 2: Focus Group Participant Demographics and Selected Responses