Neonatal Quality Improvement 1
Session: Neonatal Quality Improvement 1
065 - Use of WHO quality assessment/ quality improvement tool for gap analysis and POCQI methodology to improve Preterm Neonatal outcomes at a tertiary care centre: A Quality Improvement Initiative
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 65.6992
Sushma Nangia, Lady Hardinge Medical College & Kalawati Saran Children's Hospital, New Delhi, Delhi, India; Kiran Suthar, Lady HardingeMedical college, Delhi, Delhi, India; Pratima anand, Lady hardinge medical, New Delhi, Delhi, India; Tapas Bandyopadhyay, ABVIMS & Dr. RML Hospital, New Delhi, Delhi, India
- SN
Sushma Nangia, MD, DM (she/her/hers)
Professor
Lady Hardinge Medical College & Kalawati Saran Children's Hospital
New Delhi, Delhi, India
Presenting Author(s)
Background: Preterm birth is a leading cause of neonatal mortality and morbidity globally. Evidence suggests that over three-quarters of premature deaths can be prevented through cost-effective interventions. However, compliance with evidence-based clinical practice guidelines in neonatal care settings often falls below 50%, even in well-resourced settings. This gap can be bridged with improving adherence to good clinical practices in order to improve the outcomes in preterm neonates.
Objective: The study evaluated the system gaps related to the adherence to evidence-based practices pertaining to preterm neonates using WHO Quality Improvement tool and implemented POCQI methodology to improve and sustain the composite outcome of mortality and/or major morbidities, including bronchopulmonary dysplasia, necrotizing enterocolitis stage ≥2, late-onset sepsis, and intraventricular hemorrhage grades ≥2.
Design/Methods: The study was conducted over 14 months, using the adapted WHO QI tool for maternal and newborn Care to identify care gaps in a neonatal unit in New Delhi, India. Point of Care Quality Improvement methodology was employed to focus on key clinical practices namely kangaroo mother care, the use of mother's own milk (MOM), and antibiotic usage, utilizing multiple PDSA cycles.
Results: The WHO tool evaluated the adherence to clinical practices and showed gaps in key areas of care namely kangaroo mother care (KMC), MOM usage and antibiotic usage. Amongst 961 preterm neonates enrolled, the proportion of mothers providing KMC rose from 70.25% to 85.58%, and exclusive use of MOM by day 7 increased from 59.24% to 70.2%. Antibiotic usage declined from 25.5% to 20.67%. While process improvements were noted, the composite outcome of mortality and major morbidities did not show statistically significant reduction, though a decreasing trend was observed post-intervention.
Conclusion(s): This study demonstrated the feasibility of using WHO QI tool by trained healthcare personnel for gap analysis. POCQI is an important approach to enhance the implementation of evidence-based care practices and achieve optimal clinical outcomes for preterm neonates in resource-limited settings. Long term follow-up may be needed to observe sustenance of improvements in clinical outcomes.
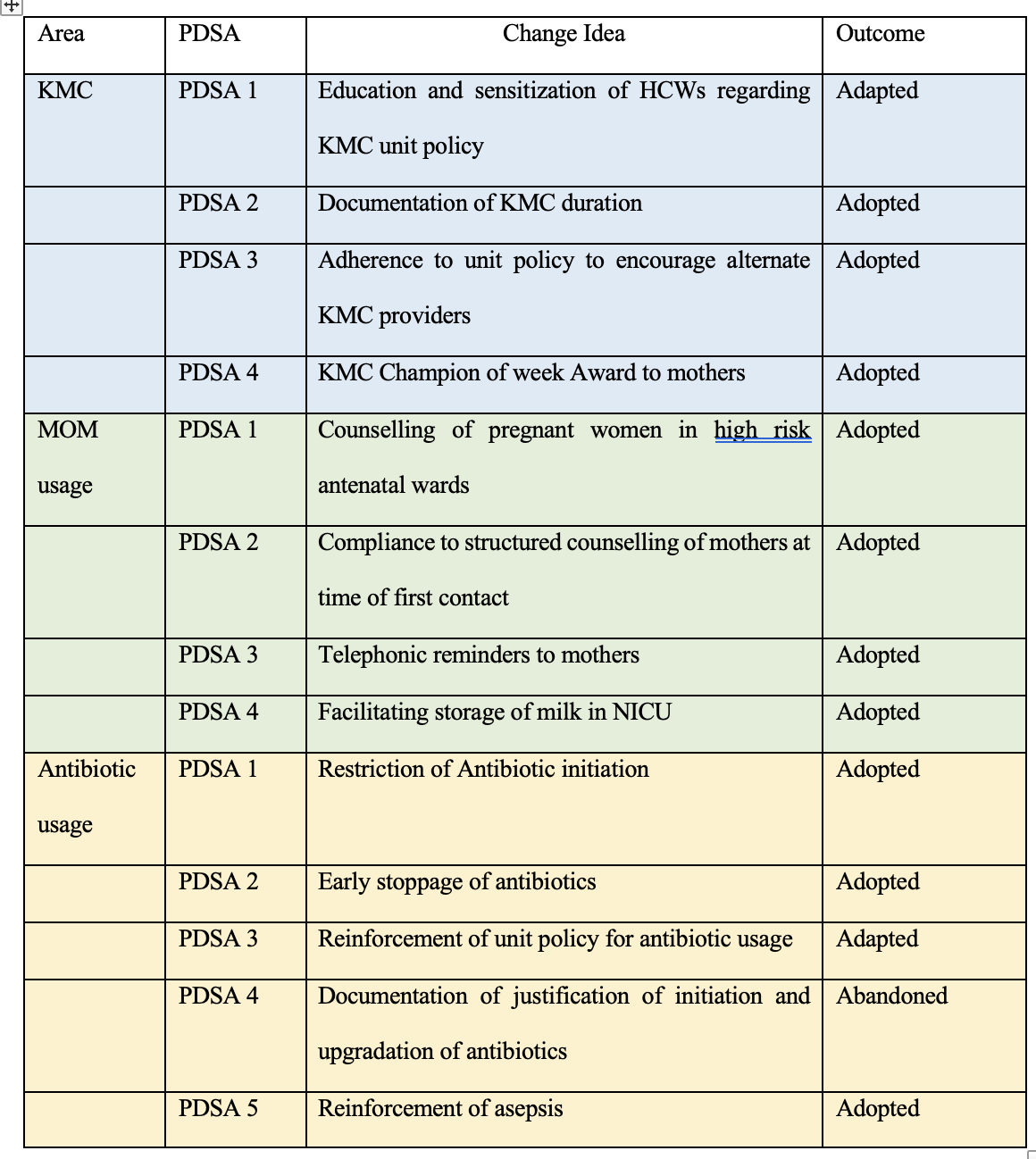
Various PDSA cycles with their outcomes
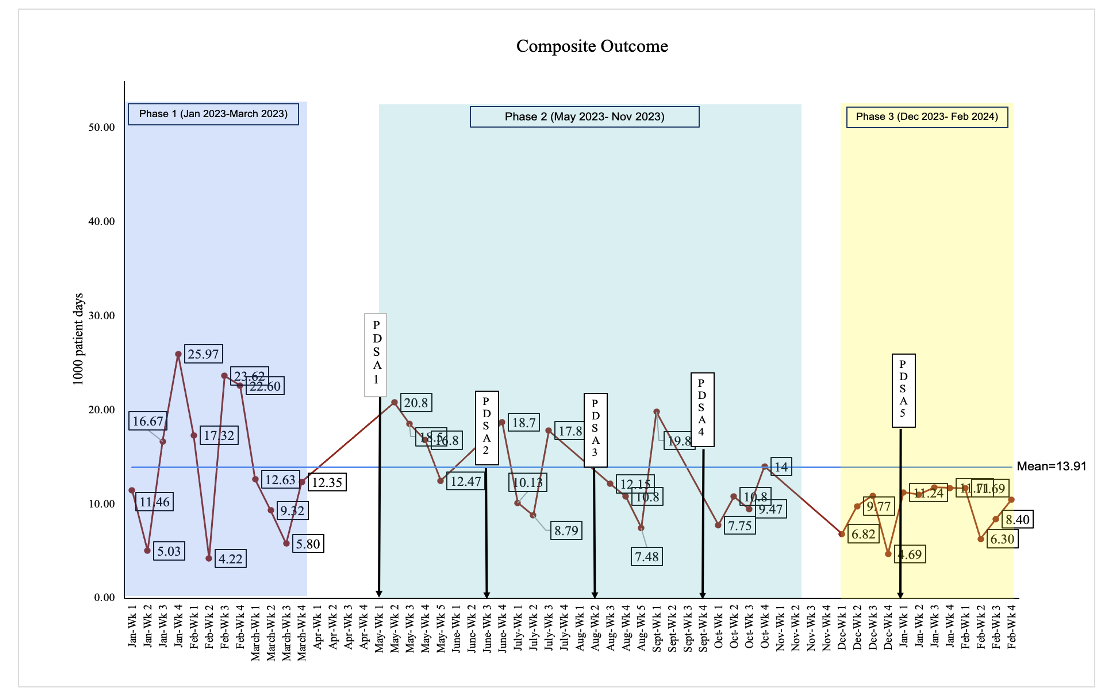
Time series run chart depicting Composite outcome / 1000 patient days
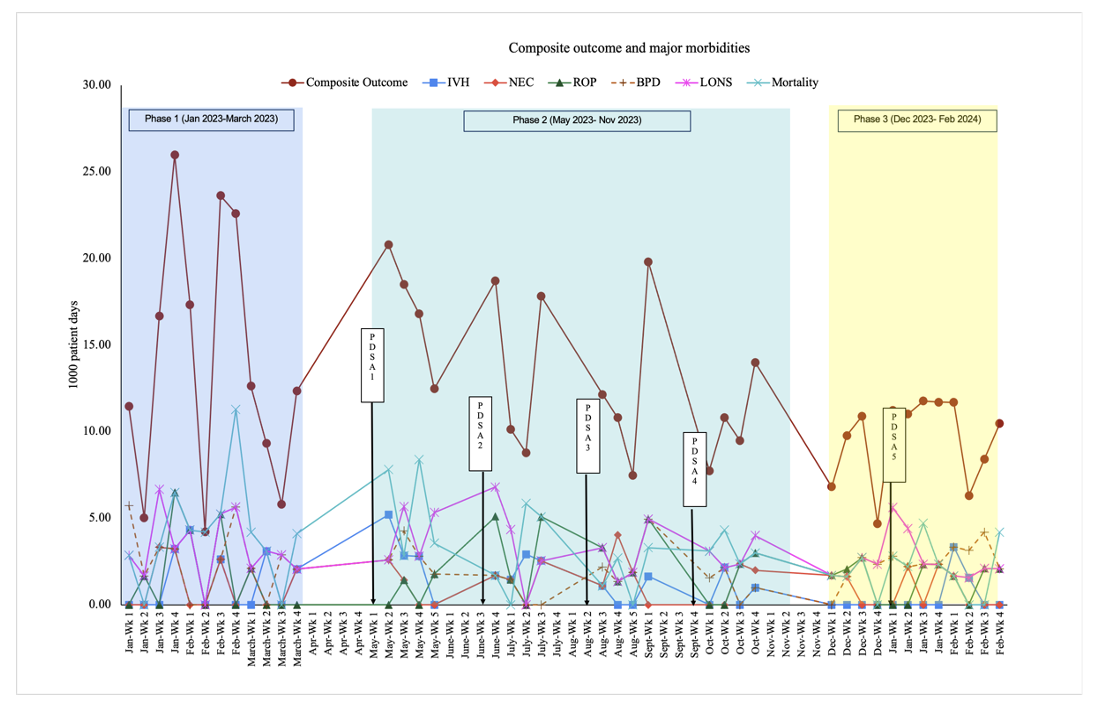
Time series run chart depicting Composite outcome and major morbidities / 1000 patient days