Neonatal Quality Improvement 3
Session: Neonatal Quality Improvement 3
093 - Quality Improvement to Reduce iatrogenic blood loss in Preterm Infants
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 93.6295
Dan Bi, Qilu hospital, Jinan, Shandong, China (People's Republic); Zenghong Huang, THE AFFILIATED HOSPITAL OF GUILIN MEDICAL UNIVERSITY, Guilin, Guangxi, China (People's Republic); Shasha Han, The First Affiliated Hospital of Jinan University, Guangzhou, Guangdong, China (People's Republic); Yan Wang, Dongguan Maternal and Child Health Care Hospital, Dongguan, Guangdong, China (People's Republic); Qi Ren, Guangzhou Women and Children’s Medical Center, Guangzhou Medical University, GuangZhou, Guangdong, China (People's Republic); Shuzheng Xu, Guangzhou Women and Children’s Medical Center, Guangzhou Medical University, Guangzhou, Guangdong, China (People's Republic); Xuwei Tao, Children's Hospital, wuhan, Hubei, China (People's Republic); Shahzeb Siddiqui, Childrens Hospital of Philadelphia, Lansdale, PA, United States; Xiaopeng Zhao, Guangzhou Women and Children's Medical Center, GuangZhou, Guangdong, China (People's Republic); John Chuo, Perelman School of Medicine, University of Pennsylvania, Doylestown, PA, United States; Huayan Zhang, Children’s Hospital of Philadelphia-University of Pennsylvania, Philadelphia, PA, United States; Canying Li, Guangzhou Women and Children’s Medical Center, Guangzhou Medical University, Guangzhou, Guangdong, China (People's Republic)

Canying Li, RN
clinical nurse
Guangzhou Women and Children’s Medical Center, Guangzhou Medical University
Guangzhou, Guangdong, China (People's Republic)
Presenting Author(s)
Background: Although frequent laboratory tests may be necessary in the care of preterm infants, these procedures pose a risk of excessive iatrogenic blood loss resulting in anemia and subsequently the need of transfusions.
Objective: We aim to mitigate iatrogenic blood loss by reduce laboratory tests in preterm infants by 10%.
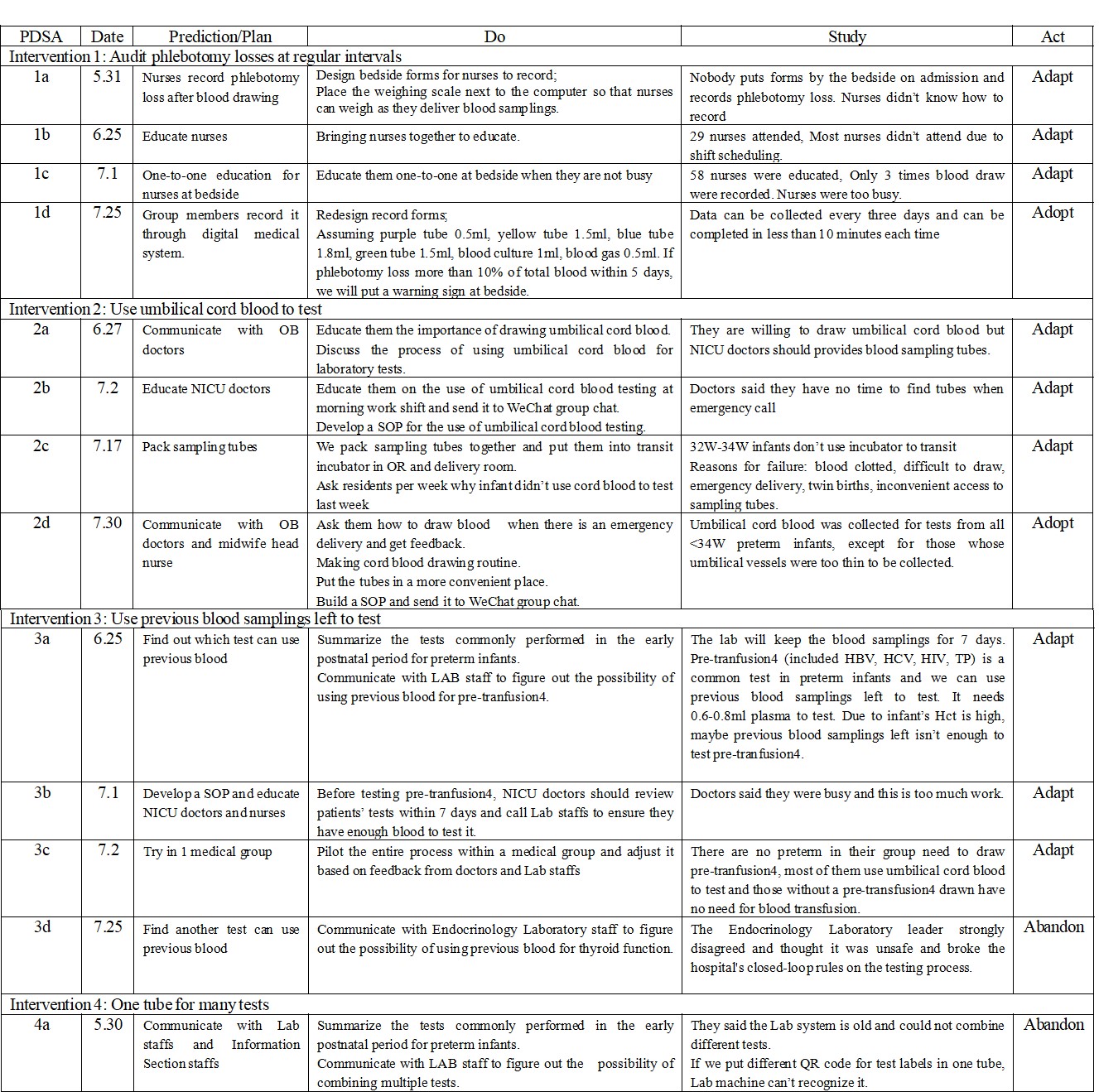
Design/Methods: A quality improvement initiative was conducted in the NICU at Guangzhou Women and Children's Medical Center from January to August 2024. Infants who were born at less than 34 weeks gestation in the first two weeks of life were included. Infants who died, with severe sepsis, or underwent exchange transfusion were excluded. Data on demographics, clinical variables, information on blood sampling, and cord blood tests were collected through the hospital's electronic medical system. Interventions included: (1) provider education to heighten the awareness of iatrogenic blood loss risks, reduce non-essential blood drawing orders and promote minimal blood sampling strategies; (2) documentation of phlebotomy-related blood loss to monitor and evaluate practices; (3) prioritization of cord blood use over venous draws when feasible; and (4) use leftover blood samples for subsequent tests when applicable. Changes in the number of blood sampling tubes used per blood testing order (as a surrogate for blood volume collected) was used as the process measure. The number of unqualified samples were recorded as the balancing measure.
Results: A total of 68 patients were included. Following the interventions, the average number of blood collection tubes decreased from 9.6 to 6 tubes (38% reduction), and most significant (48% reduction) in infants born at < 32 weeks gestation. Utility of cord blood was significantly higher (162% improvement). Meanwhile, the number of unqualified blood samples did not increase despite smaller volume of blood sampling. However, few blood tests could be performed using left-over blood samples.
Conclusion(s): By raising staff awareness, improved documentation, and increased cord blood use, our improvement team reduced blood loss from laboratory testing in preterm infants without compromising test integrity. These measures help to reduced the risk of anemia and optimize medical resource utilization. However, the low feasibility of utilizing leftover blood samples highlights the need to balance reducing blood loss with ensuring test quality during quality improvement efforts.
Control chart of sampling tubes within 2W
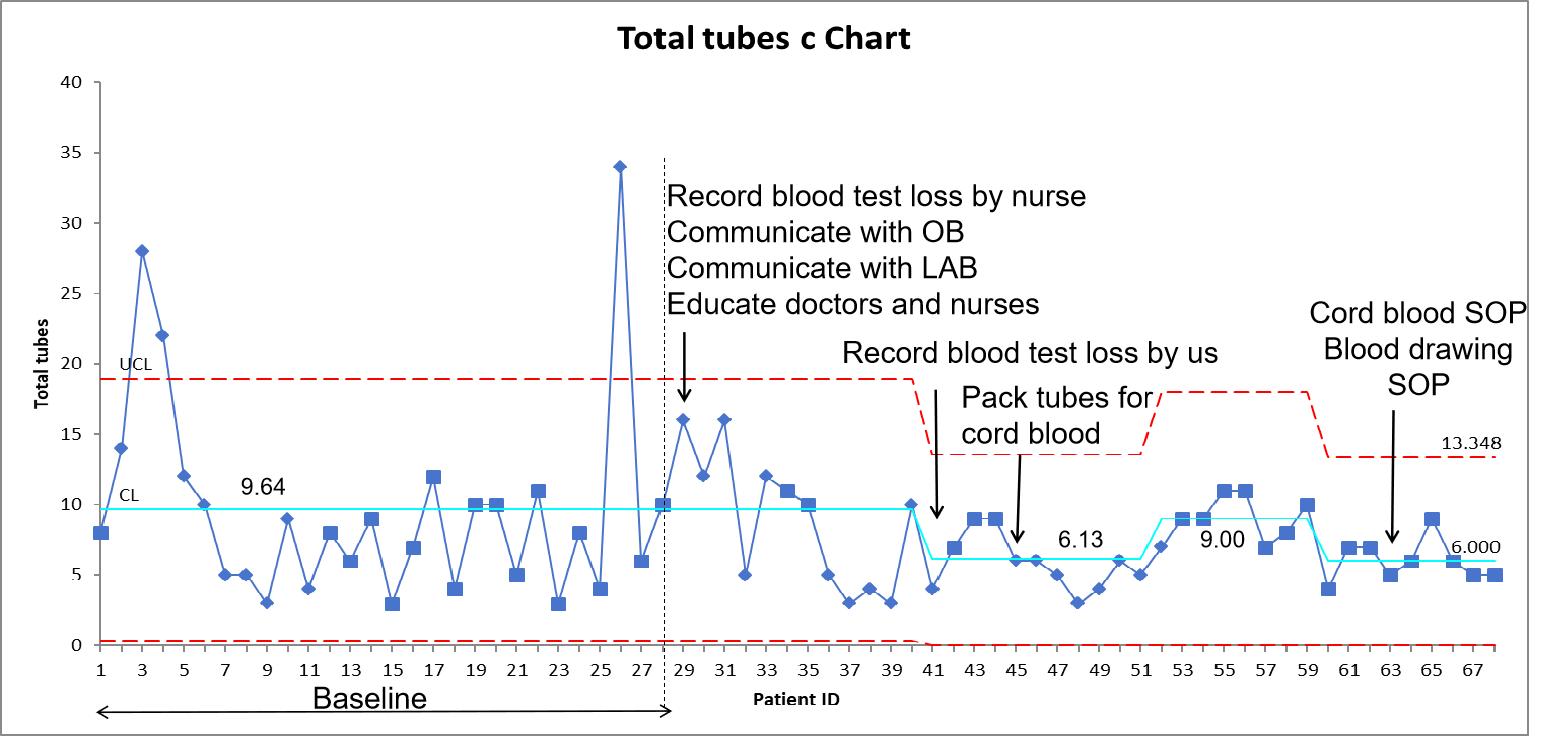
Control chart of sampling tubes within 2W categorized by gestational age
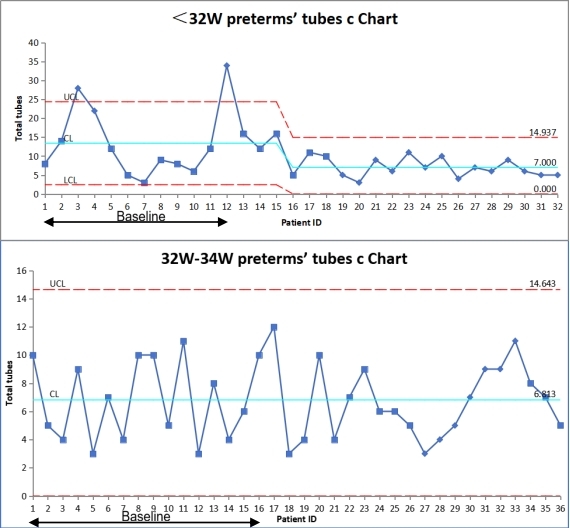
PDSA circle