Cardiology 1
Session: Cardiology 1
144 - The Clinical Impact of 3D Printing in Congenital Heart Disease
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 144.6695
Derek E. Ponce, Derek Ponce, San Francisco, CA, United States; Michael J. Bunker, UCSF Benioff Children's Hospital San Francisco, San Francisco, CA, United States; Peter Kouretas, UCSF Benioff Children's Hospital Oakland, San Francisco, CA, United States; Vinod Sebastian, UCSF Benioff Children's Hospital Oakland, San Francisco, CA, United States; Naveen Swami, University of California, San Francisco, San Francisco, CA, United States; V. Mohan reddy, University of California, San Francisco, San Francisco, CA, United States; Shafkat Anwar, University of California, San Francisco, School of Medicine, San Francisco, CA, United States

Derek E. Ponce, MD
Pediatrics Resident
UCSF Pediatrics
San Francisco, California, United States
Presenting Author(s)
Background: Congenital heart diseases (CHD) have a birth prevalence of 9.1 per 1,000 live births, and patients affected face higher morbidity and hospitalization rates compared to children with other congenital defects, according to a 2016 Heart & Lung publication by Dr. Holly Wei.
Three-dimensional (3D) printing is a rapidly advancing field that has demonstrated strong potential to improve patient care. At the field’s current state, 3D printed cardiac models can be used to represent congenital heart defects with accuracy down to the sub-millimeter scale.
Objective: Despite many advancements in medical 3D printing in the last decade, the field is still relatively new, especially in cardiac applications. Thus, we studied the accuracy and clinical utility of 3D printed cardiac models on procedural planning at our center.
Design/Methods: Study participants were patients with cardiovascular abnormalities who were candidates for catheter-based interventions or surgical repair done by pediatric cardiothoracic surgeons or interventional cardiologists/radiologists from February 2019 onward. Patients with complex anatomy were referred for 3D medical modeling to assist with surgical planning. Retrospective chart review was completed to obtain patient demographics and medical diagnosis for study participants.
3D models were printed from cardiac computed tomography angiography (CTA) using a standardized protocol. Pre-surgical planning and surgical simulation was performed by the surgeons, in consultation with a congenital heart specialist with 3D printing expertise. Surgeon feedback was collected on the anatomic accuracy and clinical impact of the models on the surgery. A Leichert scale from 0 to 5 was used to score these elements
Results: 39 patients were referred for 3D printed cardiac modeling of their anatomy for pre-surgical planning. Cases included 10 infants (mean 2.5 months), 22 pediatric cases (mean 6.4 years), and 7 adults (mean 47.5 years). The mean accuracy score provided by surgeons was 4.94 compared to intraoperative findings. For 94% of cases, surgeons reported 3D models helped understand complex anatomy or plan technical procedures. Other notable feedback included the surgeon/intervenalist’s impression that the model decreased surgical time, radiation time, and cardiopulmonary bypass time.
Conclusion(s): 3D printing is highly accurate, and provides valuable information for surgical or catheter-based interventions in patients with complex congenital heart disease. It is a robust technology with the potential to revolutionize standard of care for CHD patients of all ages.
Figure 1: 3D Model Cardiothoracic Surgeon Questionnaire
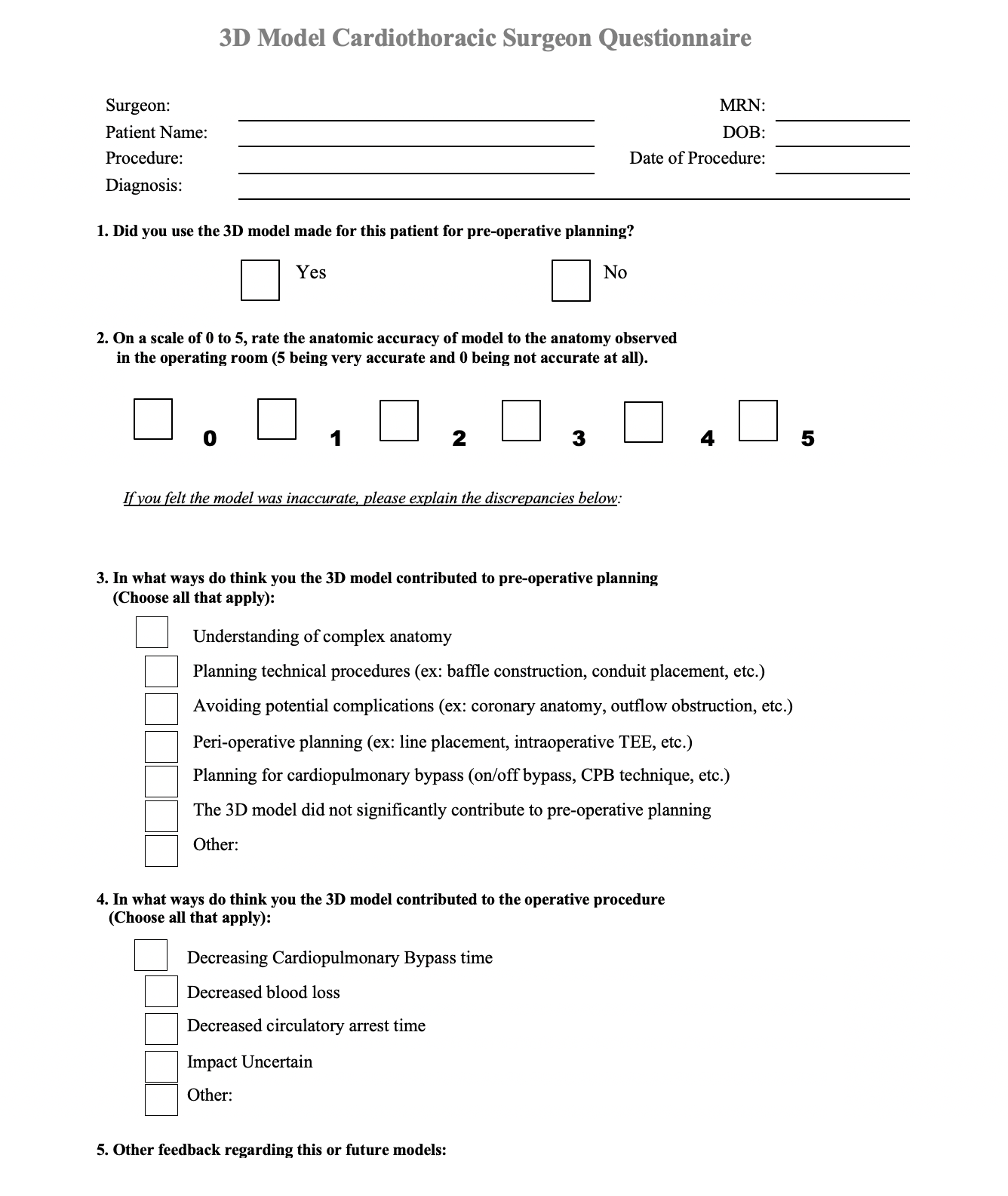
Table 1: Cardiac 3D printed cases at UCSF used for planning surgical or catheter-based procedures, February 2019 – September 2023
.png)
Table 1: Cardiac 3D printed cases at UCSF used for planning surgical or catheter-based procedures, February 2019 – September 2023
.png) Table 1 Continued
Table 1 Continued
