Emergency Medicine 1
Session: Emergency Medicine 1
409 - Advancing Pediatric Care in Community Emergency Departments: A Quality Improvement Project Focused on Emergency Diversion Strategies
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 409.3936
Keren Guterman, The University of Western Ontario - Schulich School of Medicine & Dentistry, Windsor, ON, Canada; Jonathan O’Beid, Windsor Regional Hospital, Lasalle, ON, Canada; Lisa Gawdunyk, Windsor Regional Hospital, Windsor, ON, Canada; Jonathan Foster, Windsor Regional Hospital, Windsor, ON, Canada; Jason Metcalf, Windsor Regional Hospital, Windsor, ON, Canada

Jason Metcalf, MD, PhD, FAAP (he/him/his)
Physician Lead, Pediatric Clinical Teaching Unit
Windsor Regional Hospital
Windsor, Ontario, Canada
Presenting Author(s)
Background: With increased crowding of emergency departments (EDs) across North America, there is great need for more efficient and accessible pediatric care. Canadians have markedly low access to primary care and face significant challenges accessing care on evenings and weekends. Diversion of non-emergent patients from EDs to more appropriate care settings has been proposed to improve both efficiency and quality of healthcare provided. The Pediatric Emergency Diversion Service (PEDs) was established in a community hospital in a small Canadian city of 230,000 residents to meet the need for after-hours urgent pediatric care for a regional population of over 400,000. The clinic diverts less acute patients from the ED to an on-site outpatient clinic, where a pediatrician assesses and manages the patients.
Objective: The purpose of this Quality Improvement (QI) project is to improve PEDs clinic efficacy by decreasing wait times, increasing clinic utilization rates, and reducing the number of patients leaving against medical advice (AMA).
Design/Methods: A root cause analysis (Fig. 1) was performed examining reasons for prolonged ED wait times for pediatric patients. PEDs clinic workflow was designed as follows: 1) ED triage nurses screen patients for eligibility (exclusion criteria listed in Table 1). 2) ED provider briefly assesses patient to determine safety for transfer. 3) Approved patients are relocated to the PEDs clinic for workup and management. The study team met biweekly to review quality metrics and individual patient journeys. Major interventions in the study period included extending the clinic from weekends only to a full 7-day schedule, hiring nurse practitioners to prioritize pediatric patients in the ED, and expanding clinic eligibility criteria. The impact of these interventions were analyzed by plotting quality metrics on a run chart (Fig. 2).
Results: To date, over 2,210 unique initial patient encounters have occurred in the PEDs clinic. Average total patient length of stay was reduced from 5 hours 33 minutes to 3 hours 3 minutes over the study period, and mean time from registration to provider initial assessment decreased markedly from 3 hours 34 minutes to 29 minutes. Clinic utilization increased from 70% to 92%, and the number of patients leaving AMA dropped by 33%.
Conclusion(s): This study demonstrates the feasibility and efficacy of a pediatric ED diversion program. Lessons learned may be useful for expanding this program to other areas with high ED wait times and limited pediatric after-hours care.
Table 1: Exclusion criteria for pediatric diversion from the emergency department to PEDs.
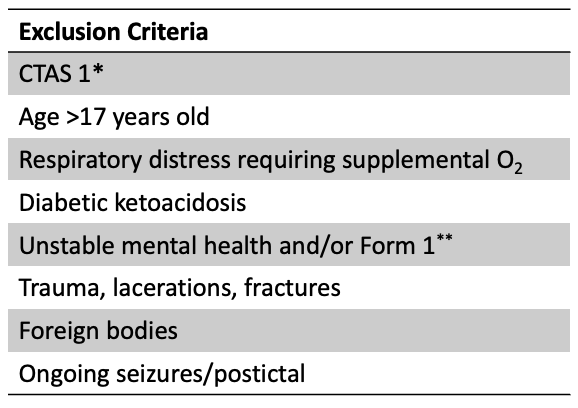 * Canadian Triage and Acuity Scale (CTAS).
* Canadian Triage and Acuity Scale (CTAS).** Form 1 allows a patient to be held in hospital for up to 72 hours to undergo psychiatric assessment.
Figure 1: Fishbone diagram illustrating the root cause analysis for excessive wait times for pediatric patients in the ED.
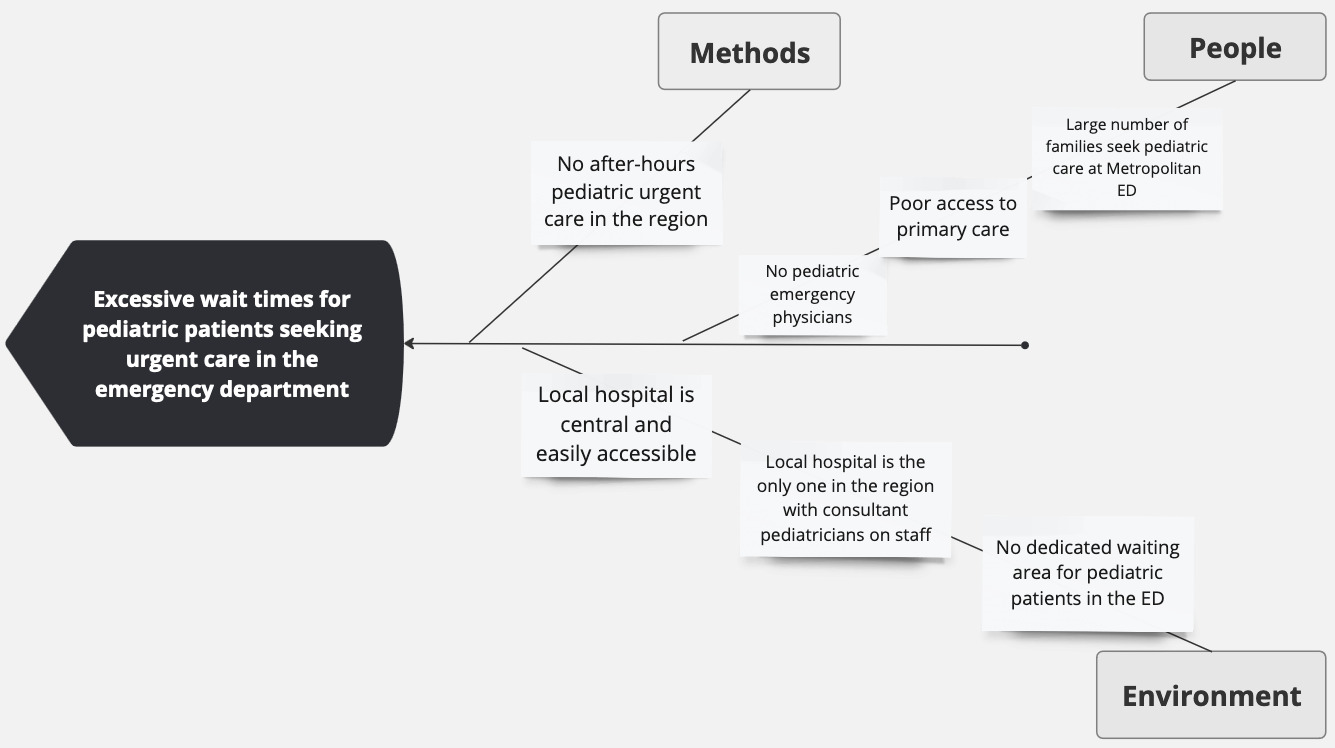
Figure 2: Run charts for quality metrics.
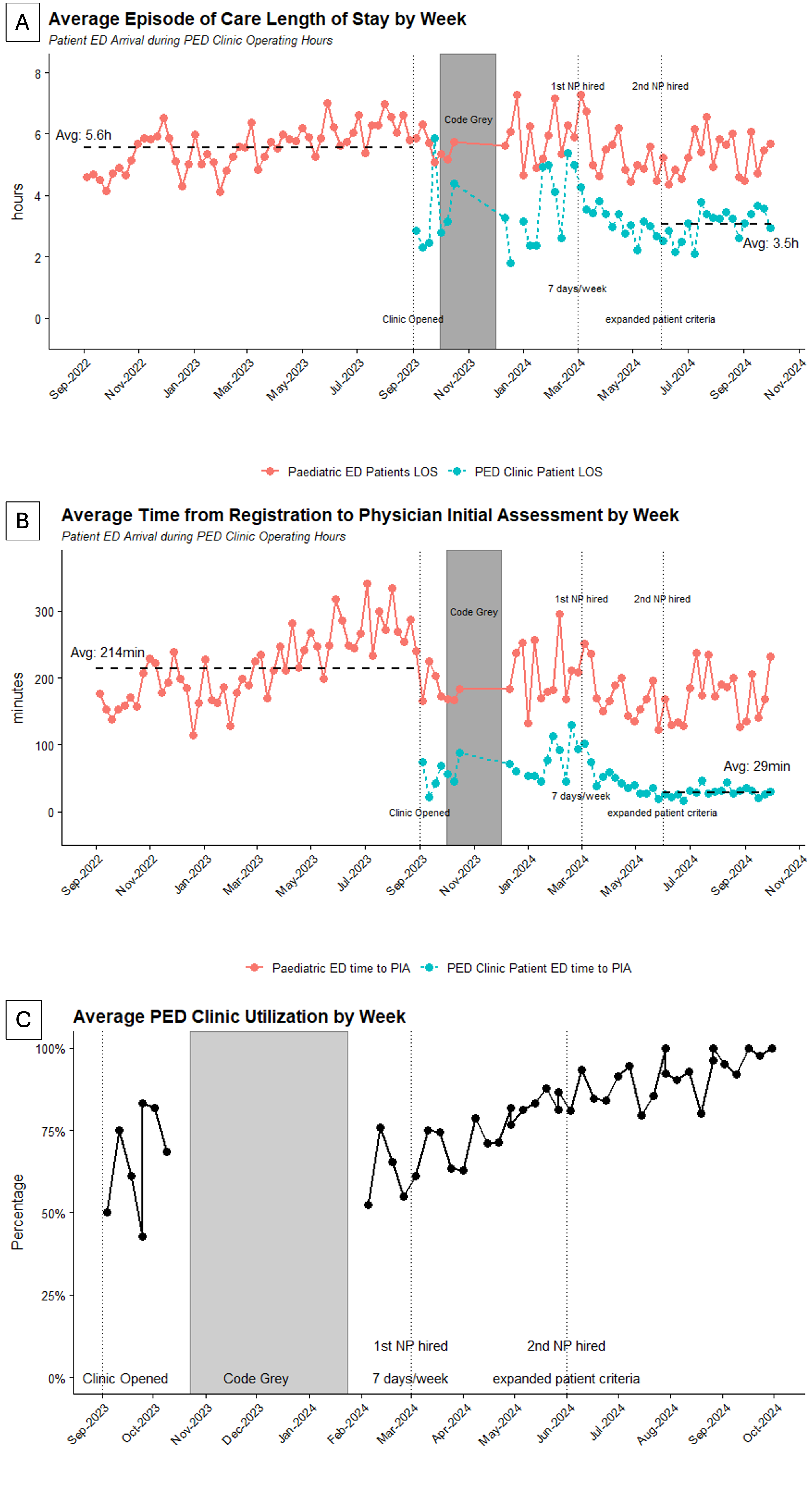 A) Average patient total length of stay by week. Code Grey indicates a period of time when hospital data systems were down and data was unable to be collected. B) Average time from registration to provider initial assessment. C) Clinic utilization rate by week, indicating the percentage of patients meeting criteria for PEDs clinic who were transferred to the clinic for assessment.
A) Average patient total length of stay by week. Code Grey indicates a period of time when hospital data systems were down and data was unable to be collected. B) Average time from registration to provider initial assessment. C) Clinic utilization rate by week, indicating the percentage of patients meeting criteria for PEDs clinic who were transferred to the clinic for assessment.

