Neonatal Quality Improvement 3
Session: Neonatal Quality Improvement 3
081 - A Quality Improvement Initiative to Reduce the Frequency of Heel Sticks in a Level IV Neonatal Intensive Care Unit
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 81.3922
Natalie Starke, University of Miami Leonard M. Miller School of Medicine, Miami, FL, United States; Chanique T. James, University of Miami Leonard M. Miller School of Medicine, Sunrise, FL, United States; Talia Kozlowski, Holtz Children's Hospital Jackson Memorial Hospital, Hollywood, FL, United States; Gretell Gomez Zaghmout, University of Miami Leonard M. Miller School of Medicine, Miami, FL, United States; Tania Fontanez-Nieves, University of Miami Miller School of Medicine, Miami, FL, United States; Laura Chavez, University of Miami Miller School of Medicine, Miami, FL, United States

Natalie Starke, MD (she/her/hers)
Neonatal-Perinatal Fellow
University of Miami Leonard M. Miller School of Medicine
Miami, Florida, United States
Presenting Author(s)
Background: Heel sticks are one of the most common invasive procedures in neonates. They often result in repeated exposure to painful stimuli, particularly within the first two weeks of life. Heel sticks are useful for various laboratory testing, the majority of which are attributed to glucose monitoring. A neonate’s developing brain is sensitive to noxious stimuli, and repeated trauma to the same area can lower their pain threshold. Skin breaking procedures have also been associated with poorer neurodevelopmental outcomes.
Objective: Our aim is to reduce the number of heel stick procedures in the first two weeks of life for all neonates admitted to the Level IV NICU at Holtz Children’s Hospital by 50% from baseline by December 2024.
Design/Methods: The electronic medical record was reviewed to obtain baseline data measuring the number of heel stick procedures within the first two weeks of life of all babies of any gestational age admitted to our level IV NICU. Neonates were included if they were admitted for greater than two weeks, and infants requiring extracorporeal membrane oxygenation (ECMO) were excluded. Data included lab investigations, point-of-care glucose testing, and blood gas analyses. Consecutive results within one hour were counted as one heel stick. In our first Plan-Do-Study-Act (PDSA) cycle, we introduced a system of combining lab investigations, blood gas analyses, and point-of-care glucose checks. This involved enlisting the cooperation of bedside nurses and respiratory therapists. In our second PDSA cycle, we are revising and standardizing the glucose monitoring policy in the NICU and will provide further education to nursing and respiratory staff to ensure consistent implementation.
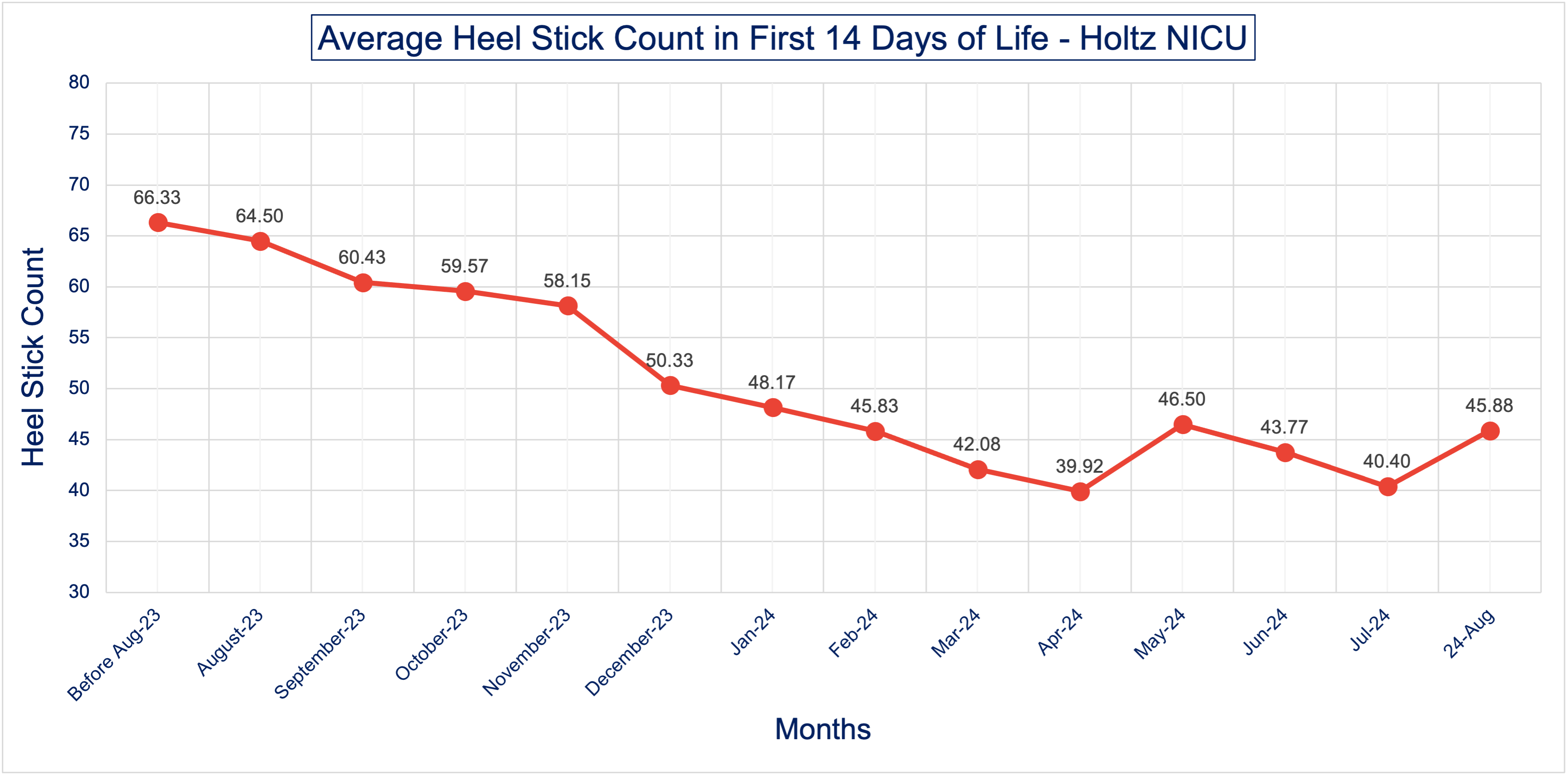
Results: Data were collected from 36 neonates from August to November 2023 to establish a baseline number of heel sticks for the unit. Data were then collected from 104 neonates from December 2023 to August 2024 following the implementation of PDSA Cycle 1. The average number of heel sticks per neonate in the first two weeks of life declined by 25% (Figure 1), with the average number in the baseline cohort of 60.6 (SD ± 13.57) decreasing to 44.16 (SD ± 12.18) following implementation of PDSA Cycle 1. This data demonstrates a reduction in repeated painful heel sticks over time in our NICU (Figure 2)
Conclusion(s): There was a decrease in the number of heel stick procedures in our NICU after our focused interventions. We will continue to reinforce the practices we have enacted as well as work towards achieving our goal reduction in our upcoming PDSA cycles.
Figure 1: Run Chart of Mean Heel Stick Count in First 14 Days of Life
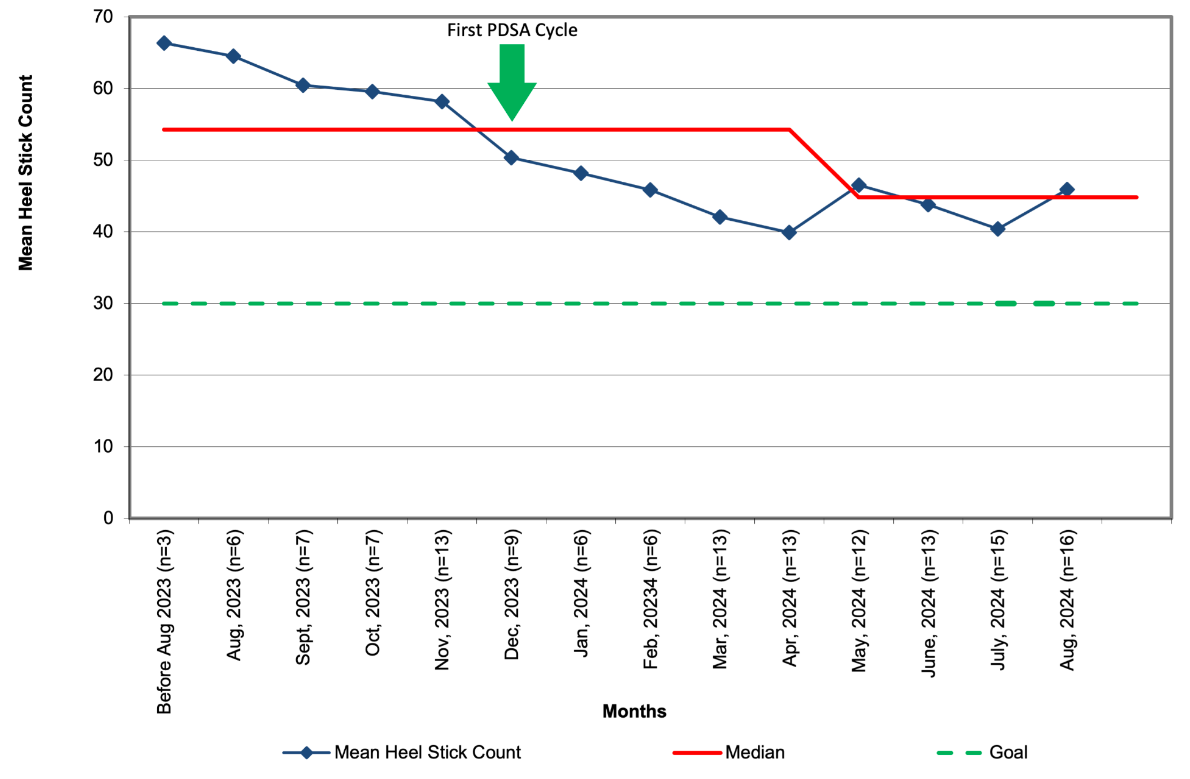
Figure 2: Average Heel Stick Count in the First 14 Days of Life