Quality Improvement/Patient Safety 2
Session: Quality Improvement/Patient Safety 2
017 - Analysis of Poison Center Pediatric Health Care Facility Referral Refusals: Data from the National Poison Data System (2009-2023)
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 17.3897
Anna Zmuda, University of Virginia School of Medicine, Charlottesville, VA, United States; Sage Timberline, University of Virginia, Charlottesville, VA, United States; Rita Farah, University of Virginia School of Medicine, CHARLOTTESVILLE, VA, United States; Jennifer R Charlton, University of Virginia School of Medicine, charlottesville, VA, United States; Nathan P. Charlton, University of Virginia School of Medicine, Charlottesville, VA, United States
- ST
Sage Timberline, MD
Fellow
University of Virginia
Charlottesville, Virginia, United States
Presenting Author(s)
Background: Approximately 1.1 million cases of xenobiotic exposures in persons ≤19 are called to United States (US) Poison Centers (PC) each year, representing roughly half of all PC cases. The majority of cases are unintentional exposures and 78% of these cases are managed at home, with 22% referred to the hospital for evaluation. Less than 2% of all PC callers refuse referral to a health care facility (HCF) when advised to do so by the PC, but less is known about the pediatric population.
Objective: This study aimed to identify number of yearly pediatric HCF referral refusals and to characterize the xenobiotics most often associated.
Design/Methods: This was a retrospective study of pediatric reports to the US National Poison Data System over a 15-year period from January 1st, 2009 to December 31st 2023. The NPDS was queried for single-substance exposures via all exposure routes in patients ≤19 years old. We assessed total number of patients, age and the xenobiotics involved.
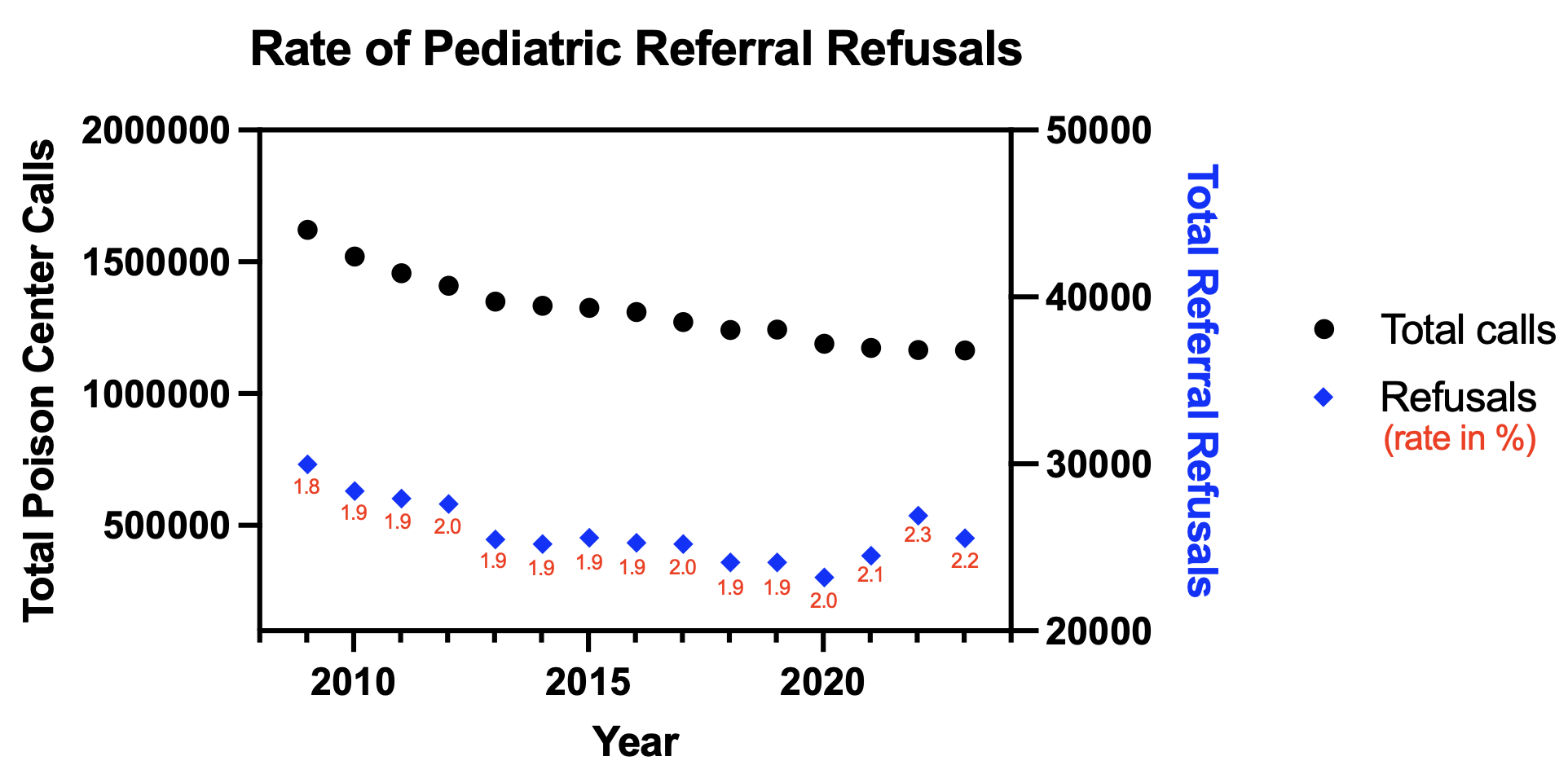
Results: Over the study period there were 152,485 calls (average 10,165 yearly) in which callers refused referral to a HCF. The peak number of refusals was 14,954 in 2009, with a low of 7,895 in 2023. However, total yearly PC calls declined over the study period, so the rate of refusal remained fairly consistent, ranging from 1.8-2.3% with an average of 2.0% overall. Referral was refused most commonly for teenagers (13-19), with an average of 3305 (32%) refusals yearly, followed by age 2 (n=1904, 19%) and age 1 (n=1650, 16%). Acetaminophen products (418 cases yearly, 4%) were the single substance most often associated with refusal, followed by ibuprofen (n=377, 4%) and miscellaneous unknown drugs (n=344, 3%). The main cause of exposure was unintentional (n=104,913, 45%), followed by suspected suicide (n=22,290, 15%). Vomiting was the symptom most often associated with refusal (10% of cases) and drowsiness/lethargy comprised 6% of cases.
Conclusion(s): While total number of pediatric refusals to HCFs declined over the 15-year period, the rate remained relatively stable. Unintentional exposures to relatively innocuous medications may not require further follow up by PC staff. However, suspected suicide, comprising 15% of cases, and cases involving dangerous xenobiotics such as acetaminophen, comprising 4% of cases, require more PC and first responder services, such as welfare checks. There were a large variety of agents involved, with no single agent making up than 4% of the total. Additional work is needed to determine the reasons for refusal to HCFs, outcomes and whether PC training interventions would decrease the rate of refusal.
Rate of Pediatric Referral Refusals