Emergency Medicine 1
Session: Emergency Medicine 1
407 - A Pilot Pediatric Clinical Decision Unit Improves Emergency Department Throughput While Maintaining Quality Balancing Measures
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 407.3887
Sebrina D. Perkins, Baylor College of Medicine, San Antonio, TX, United States; Britney Fletcher, CHRISTUS Children’s Hospital, San Antonio, TX, United States; Diana M. Sestito, CHRISTUS Children’s Hospital, San Antonio, TX, United States; Megan O'Brien, Baylor College of Medicine, San antonio, TX, United States; Carly Hinojosa, Baylor College of Medicine, Boerne, TX, United States; Heather Borowiec, Baylor College of Medicine, San Antonio, TX, United States; Alyssa OCana, CHRISTUS Children’s Hospital, San antonio, TX, United States; Julie Vereen, CHRISTUS Children's, San Antonio, TX, United States; Monica Gutierrez, CHRISTUS Children’s, San Antonio, TX, United States; Kelly Jackson, Children's Hospital of San Antonio, FLORESVILLE, TX, United States; Lawrence Quang, Baylor College of Medicine, San Antonio, TX, United States

Sebrina D. Perkins, MD (she/her/hers)
Pediatric Emergency Medicine Faculty
Baylor College of Medicine
San Antonio, Texas, United States
Presenting Author(s)
Background: Nationwide, children's hospitals face challenges with Emergency Department (ED) overcrowding and limited inpatient bed capacity, while trying to reduce healthcare costs. Since the 1960's, Clinical Decision Units (CDUs) have provided a safe alternative for short term care ( < 24 hours) in the ED and are considered a best practice by the American College of Emergency Physicians (ACEP). Though commonly adopted by adult EDs, only 14 children's hospitals report having a CDU. Sparse published experience is available about pediatric CDU operations and outcomes.
Objective: We sought to develop and implement a new 4-bed, Type 1 pediatric CDU (dedicated space and defined protocols) to improve ED throughput metrics, while maintaining quality balancing measures.
Design/Methods: A CDU Implementation Committee of ED physicians, nurses, advanced practice providers (APPs), and hospital administrators, consulted with CDU medical directors from 3 established pediatric CDUs, and their best practices and protocols were adapted to our local ED setting. Dedicated nurses and APPs, with supervision by the shift attending physician, cared for CDU patients in a specific ED pod with defined protocols. CDU throughput outcome measures were ED admission hold hours, % patients left without being seen (LWBS), and admission/discharge length of stay (LOS). Quality balancing measures were CDU % discharged, % admitted, % needing a rapid response, and % return to ED within 72 hours of discharge.
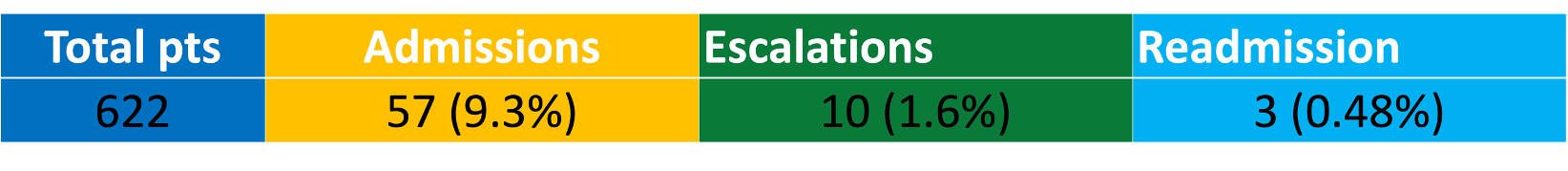
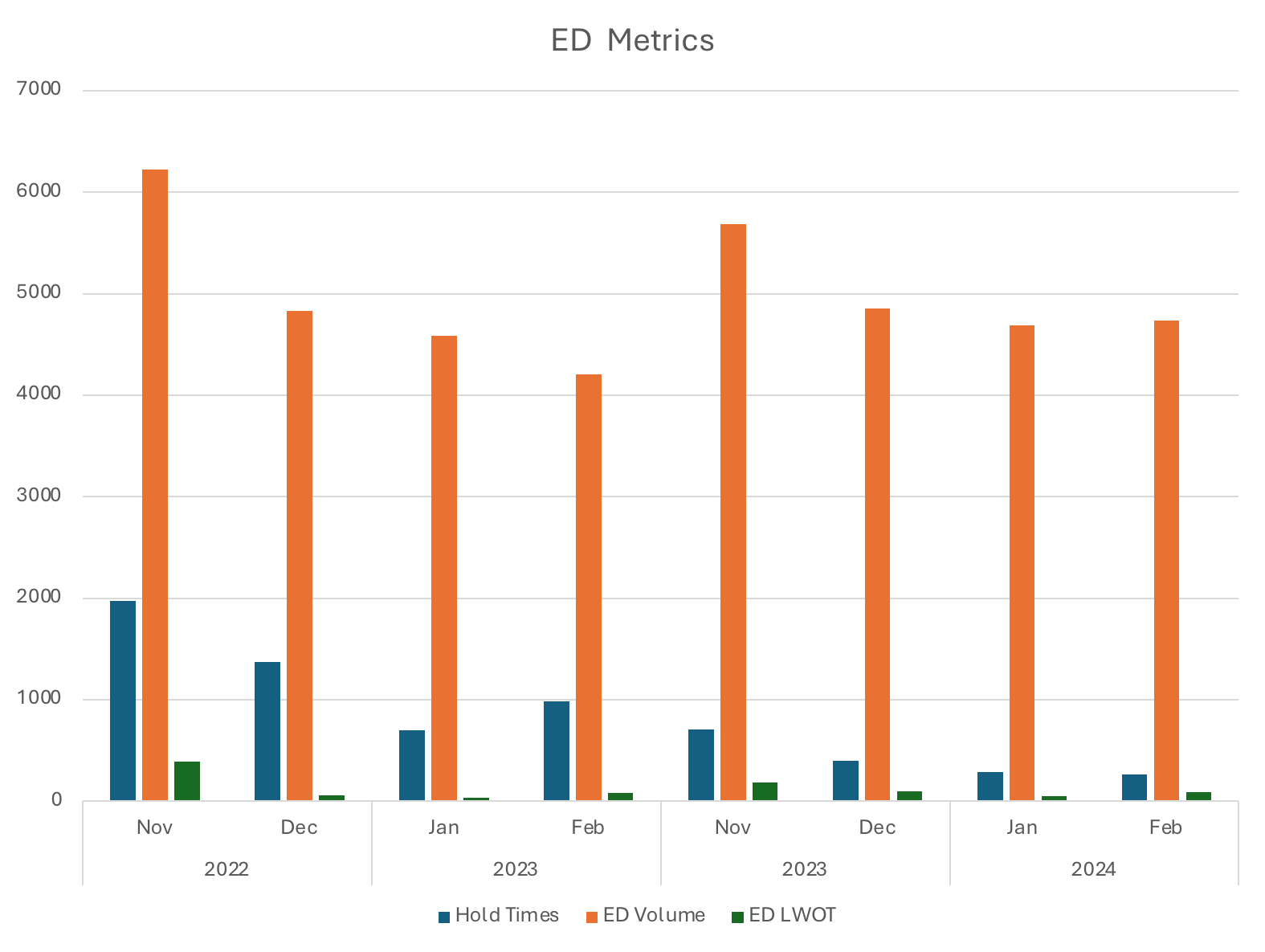
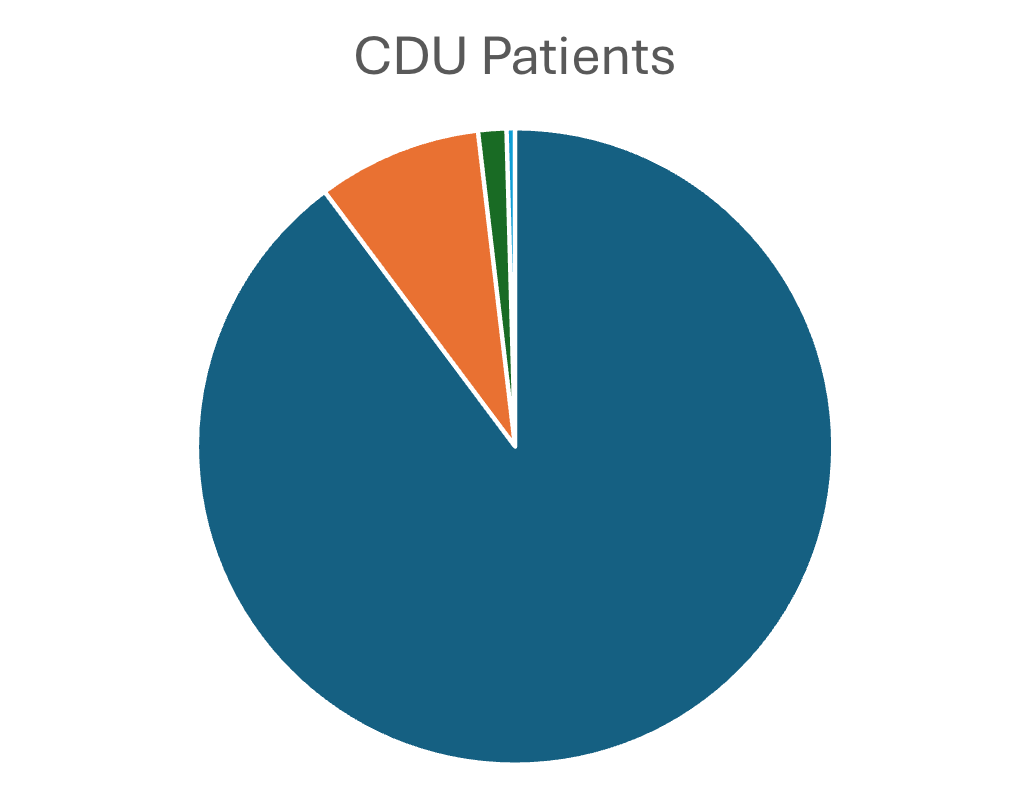
Results: From December 2023 - August 2024, 622 patients were admitted to the CDU. Compared to the previous year, ED admission hold hours decreased by 58%, LWBS decreased from 2.8% to 2.1%, and admission/discharge LOS decreased by 21 and 26 minutes, respectively. The CDU discharge rate was 91%, admission rate 9%, rapid response rate 1.6%, and 72-hour discharge return rate 0.5%.
Conclusion(s): ACEP, the American Academy of Pediatrics, and the National Academy of Medicine support the placement of appropriate ED patients in observation areas like CDUs, rather than inpatient beds. CDUs have been implemented in about 1/3 of adult EDs across the country. The published adult CDU literature indicates CDU efficacy; yet most children's hospitals haven't implemented CDUs. Virtually, no pediatric CDU throughput and quality outcomes are tracked or reported. Adult CDUs generally admit 20% and discharge 80% of patients with a 10% return rate. Our pilot pediatric CDU throughput and quality outcomes exceed adult CDU reported metrics, supporting the notion that a pediatric CDU may avoid unnecessary admissions, optimize inpatient bed capacity, and improve ED throughput.
ED Hold Hours/ ED Volume/ ED LWBS
Inpatient Admission Rate/ Escalation Rate/ Readmission Rate
Inpatient Admission Rate/Escalation Rate/Readmission Rate