Infectious Diseases 1: Atypical and unusual infections
Session: Infectious Diseases 1: Atypical and unusual infections
609 - Disseminated Cat-Scratch Disease Mimicking MIS-C
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 609.4211
Sung Hwan Choi, University of Hawaii, John A. Burns School of Medicine, Honolulu, HI, United States; Rodolfo Bégué, University of Hawaii, John A. Burns School of Medicine, Honolulu, HI, United States

Sung Hwan Choi, MD (he/him/his)
Resident
University of Hawaii, John A. Burns School of Medicine
Honolulu, Hawaii, United States
Presenting Author(s)
Background: Multisystem inflammatory syndrome in children (MIS-C) continues to be reported. Diagnosing MIS-C requires ruling out alternative diagnoses, and treatment involves immunomodulating agents. Consequently, excluding infectious causes is crucial, as misdiagnosis could lead to administering immunomodulating agents to patients with infections. However, MIS-C has become less severe, with fewer than half of the patients presenting with shock, making it more challenging to differentiate MIS-C from other etiologies.
Objective: We report a patient who initially met the clinical and laboratory criteria for MIS-C but was later diagnosed with disseminated cat-scratch disease (CSD).
Design/Methods: This is an Institutional Review Board (IRB)-exempt retrospective chart review of a single patient.
Results: A 12-year-old female presented with an eight-day history of fever, a five-day history of evanescent skin rashes, and a two-day history of watery diarrhea. At fever onset, the patient experienced generalized abdominal pain, myalgia, and photophobia, which resolved within a few days. Also, the patient developed reddened, cracked lips and a pinpoint conjunctival erythema in her right eye during the course of her illness. The patient had tested positive for coronavirus disease 2019 (COVID-19) three weeks prior to fever onset. The patient had been scratched by a cat after the onset of fever. On examination, mild injection to bilateral temporal conjunctivae and a few macular rashes on her lower abdomen were noted. Laboratory test results are shown in Table 1. Given the patient’s uncharacteristically well appearance for a presumed MIS-C case and persistent abdominal symptoms, an abdominal ultrasound was performed, revealing hepatomegaly and multiple ill-defined hypoechoic lesions in the liver and spleen, suggestive of disseminated cat-scratch disease. This finding was further confirmed with contrast-enhanced abdominal computed tomography (Images 1 and 2). Ophthalmologic examination showed bilateral neuroretinitis. Echocardiography revealed normal left ventricular ejection fraction with no coronary artery dilatation. The patient was empirically treated with rifampin and doxycycline, with a good response. Bartonella henselae antibodies were later found to be positive, with high titers. A follow-up ophthalmologic examination showed resolution of optic disc edema.
Conclusion(s): Disseminated cat-scratch disease should be considered as a differential diagnosis when MIS-C is suspected, especially in endemic regions. Radiographic evaluation of the abdomen can be helpful in diagnosis if the clinical presentation is inconclusive.
Table 1.
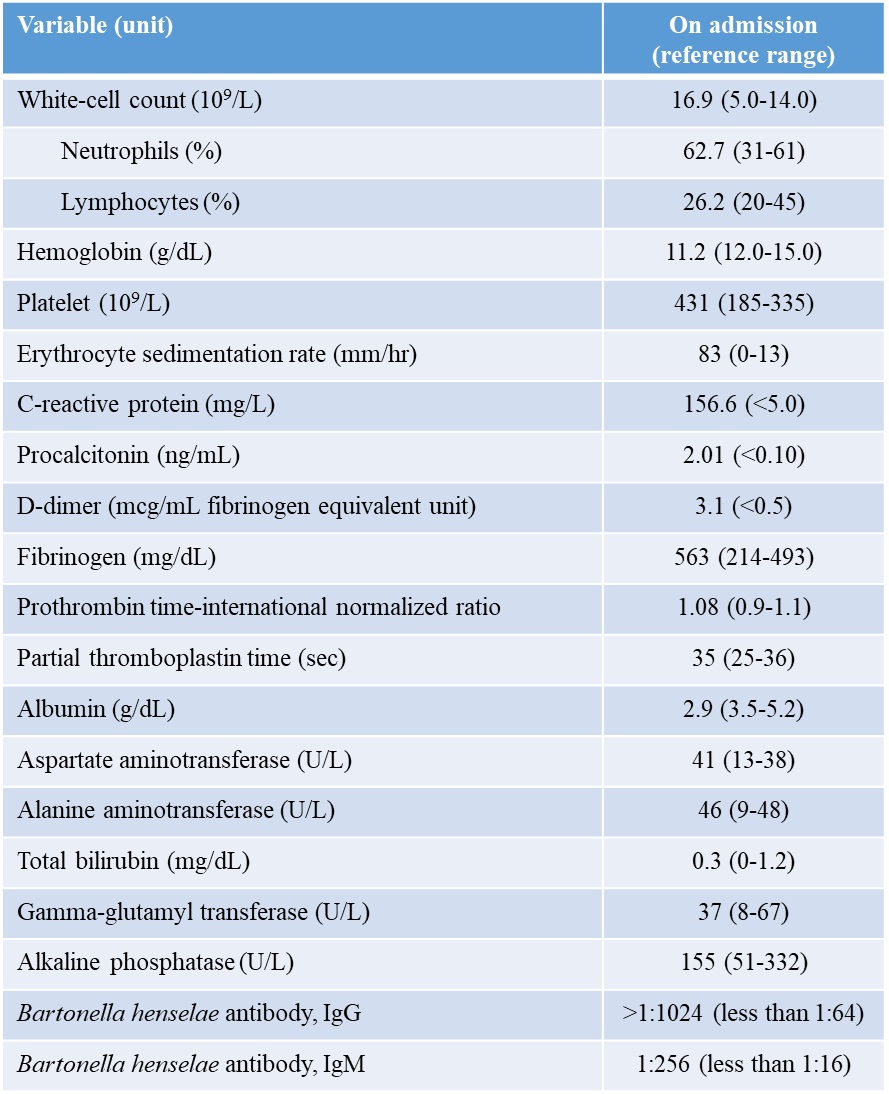 Laboratory Results
Laboratory ResultsImage 1.
 A contrast-enhanced computed tomography scan of the abdomen and pelvis revealed a few scattered sub-centimeter hypodense lesions in the liver and spleen.
A contrast-enhanced computed tomography scan of the abdomen and pelvis revealed a few scattered sub-centimeter hypodense lesions in the liver and spleen.Image 2.
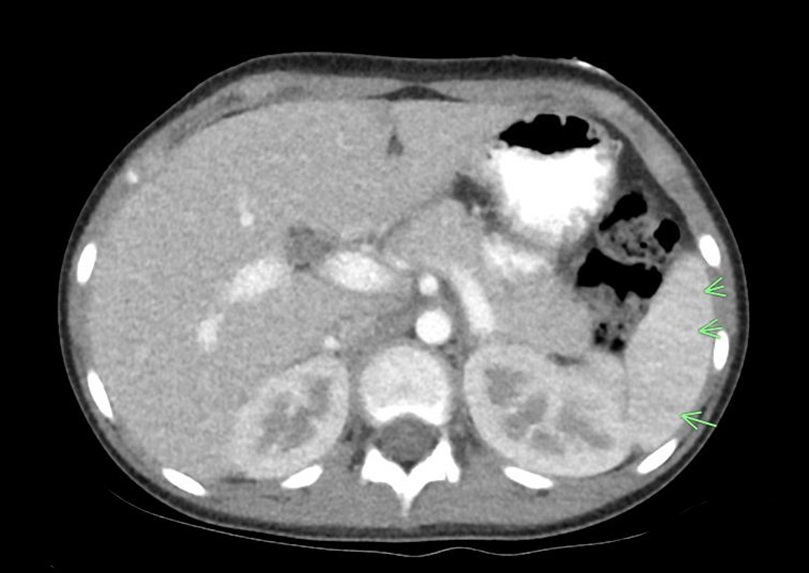 A contrast-enhanced computed tomography scan of the abdomen and pelvis revealed a few scattered sub-centimeter hypodense lesions in the liver and spleen.
A contrast-enhanced computed tomography scan of the abdomen and pelvis revealed a few scattered sub-centimeter hypodense lesions in the liver and spleen.
