Cardiology 3
Session: Cardiology 3
163 - CHNC Center Variability in Management of Patent Ductus Arteriosus: Analysis of Clinical Practice Guidelines
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 163.4549
Sharada H. Gowda, Baylor College of Medicine, Houston, TX, United States; Mark F. Weems, University of Tennessee Health Science Center College of Medicine, Memphis, TN, United States; Rakesh Rao, Washington University in St. Louis School of Medicine, St. Louis, MO, United States; Shawn Sen, CHOC Children's Hospital of Orange County, irvine, CA, United States; Shannon Hamrick, Emory University School of Medicine, Atlanta, GA, United States; Philip Levy, Boston Children's Hospital, BROOKLINE, MA, United States; Ayan Rajgarhia, CHOC Children's Hospital of Orange County, Orange, CA, United States; Molly K. Ball, Nationwide Children's Hospital, Columbus, OH, United States; Sarah Keene, Emory/Childrens Healthcare Of Atlanta, Decatur, GA, United States

Sharada H. Gowda, MD, FAAP (she/her/hers)
Associate Professor of Pediatrics
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: Diagnostic criteria and management of hemodynamically significant patient ductus arteriosus (hsPDA) has evolved over time. There is lack of standardized diagnostic criteria, controversy around optimal mode of therapy, and timing of interventions. To address this gap, individual centers develop clinical practice guidelines.
Objective: To collate existing PDA guidelines among CHNC centers and explore diagnostic and therapeutic approach to management of an hsPDA.
Design/Methods: We sent an email requesting PDA guidelines to CHNC center representatives. We assessed guideline for description of the included population, definition of hs PDA (clinical and echocardiographic criteria), options for conservative management, use of prophylactic medication, early therapy, rescue therapy, medication dosing, and criteria for definitive closure. We used descriptive analytics to present the data.
Results: Thirty-eight of 44 CHNC centers (86%) responded. Clinical signs of the PDA are mentioned by 18 centers (72%) and 21 centers (84%) describe echocardiographic diagnostic criteria of an hsPDA. Most commonly used echo criteria included the ductal size, isovolumic relaxation time, left atrium to aorta ratio, flow reversal in descending aorta. Few centers used flow reversal in celiac trunk, and middle cerebral artery.
Ten of 25 centers (40%), addressed conservative management including fluid restriction, PEEP increase, maintaining a hemoglobin level >12 mg/dl, and diuretic use. Five centers (20%) recommend prophylactic indomethacin in select infants. Thirteen of 25 centers (52%) use early pharmacologic therapy in the first week after birth, while 10 centers (40%) use it beyond the first week. Pharmacotherapy was addressed by 24 of 25 centers (96%). While 4 (16%) offer no preference of medication, Ibuprofen is the most recommended first-line therapy, recommended by 13 centers (52%), Indomethacin is first-line therapy at 2 centers (8%), and acetaminophen is first-line therapy at 4 centers (16%). while 23 of 25 centers (92%) mentioned Transcatheter closure, while 12 of 25 (48%) centers addressed surgical ligation.
Conclusion(s): Despite center variability, two third CHNC centers have a PDA management guideline. Ibuprofen is the most common first-line therapy; followed by acetaminophen and indomethacin. Most centers have incorporated pertinent echocardiogram criteria to define an hsPDA with stepwise approach of initial medical management and definitive transcatheter PDA closure into the guideline. Additionally, there is a shift in definitive closure practice from surgical ligation to transcatheter approach.
CHNC PDA Therapy
.jpg) Timing of screening, Medication choices , and Maximum course
Timing of screening, Medication choices , and Maximum coursePDA echo criteria
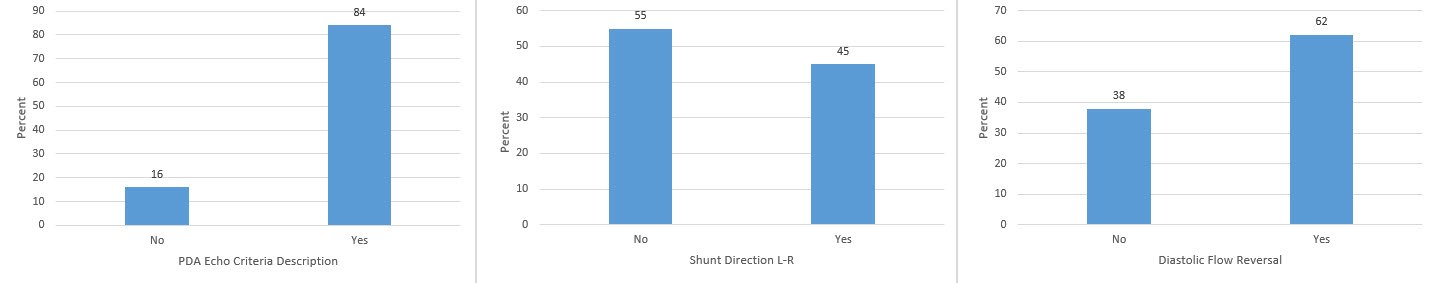 Echo criteria, Shunt direction, and Diastolic flow reversal
Echo criteria, Shunt direction, and Diastolic flow reversal
