Infectious Diseases 1: Atypical and unusual infections
Session: Infectious Diseases 1: Atypical and unusual infections
608 - Clinical Characteristics, Management, and Outcomes of Mycoplasma pneumoniae-associated Reactive Infectious Mucocutaneous Eruption (RIME)
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 608.4486
Guliz Erdem, Nationwide Children's Hospital, columbus, OH, United States; Hassan El Chebib, Connecticut Children's Medical Center, Hartford, CT, United States; Kaya Ceyhan, Ohio State University College of Medicine, Columbus, OH, United States; Pablo J. Sanchez, Nationwide Children's Hospital -OSU, Columbus, OH, United States; Ian C.. Michelow, Connecticut Children's and University of Connecticut School of Medicine, Hartford, CT, United States
- GE
Guliz Erdem, MD (she/her/hers)
Professor
Nationwide Children's Hospital
columbus, Ohio, United States
Presenting Author(s)
Background: Since late Spring 2024, the CDC has observed increasing rates of Mycoplasma pneumoniae (Mp) respiratory infections, especially among children. In addition to increasing rates of Mp positive test results as high as 35%, we have observed an unprecedented surge of cases with Mp-associated Reactive Infectious Mucocutaneous Eruption (RIME).
Objective: To characterize the demographics, clinical characteristics, laboratory findings, management and outcomes of children and adolescents with Mp-associated RIME.
Design/Methods: This is a retrospective chart review of children hospitalized at Nationwide Children's Hospital in Columbus, OH and Connecticut Children's in Hartford, CT since June 2024. Patients were included if they had concurrent or recently resolved lower respiratory disease, active mucositis, and a positive Mp PCR assay from an upper respiratory tract sample and/or positive serum Mp IgM and/or IgG.
Results: Thirteen consecutive patients (54% males; 54% from CT), ranging in age from 1.9 to 17 years (69% >= 12 years of age) were diagnosed with Mp-associated RIME within a 5-month timeframe. HSV PCR testing was performed in 62% of cases and all were negative. No patients had proven coinfections with other respiratory viruses or bacteria. Nine (69%) had radiologic features of pneumonia, 3 (23%) of whom required oxygen and 1 (8%) received ICU care. Extra-pulmonary manifestations involved the oral mucosa (92%), conjunctiva (85%), urethra (46%) and skin (38%) with multiple concurrent sites frequently affected. Preceding symptoms lasted 2-12 days (mean, 6 days). Mean maximum temperature within 24 hours of admission was 38.1 degrees Celsius and mean maximum CRP within 48 hours was 7.0 mg/dL. Twelve (92%) patients were treated with steroids and all patients received azithromycin or doxycycline before or during admission. Mean length of hospitalization was 9.5 days (range 3-24 days as of current date; 3 still hospitalized). Neutrophil: Lymphocyte Ratio (NLR) >5.0 within 24 hours of admission was associated with significantly higher CRP within 48 hours of admission (P=0.02; Figure 1) and longer hospitalization (P=0.01; Figure 2).
Conclusion(s): The recent global and national re-emergence of Mp respiratory disease has been associated with RIME requiring hospitalization in OH and CT. The majority of cases were teenagers, almost one-quarter required oxygen, and multiple mucocutaneous sites were involved. NLR >5.0 was associated with prolonged hospitalization and may be a useful predictive biomarker for length of stay. Prospective studies are needed to evaluate the effectiveness of steroids and antibiotics.
Figure 1. Comparison of CRP values in children with Mycoplasma pneumoniae-associated RIME stratified by Neutrophil:Lymphocyte Ratios
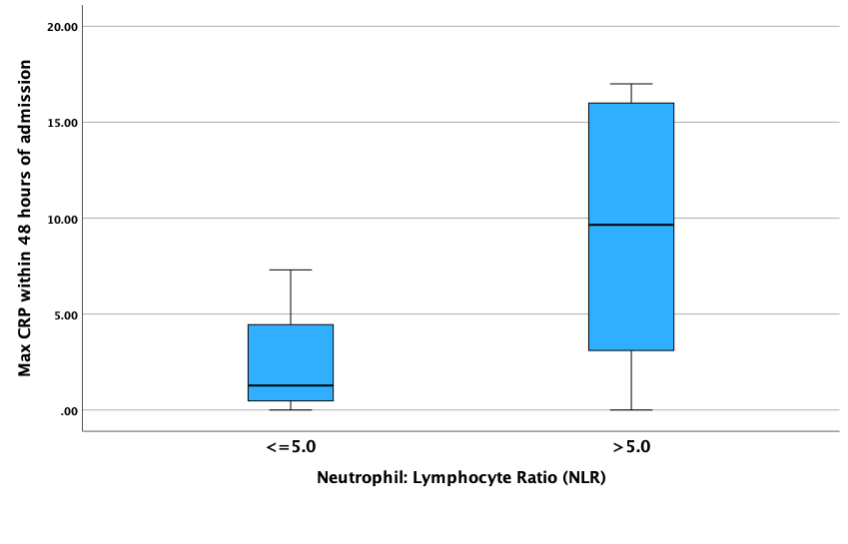 CRP < 0.5 mg/dL is considered normal.
CRP < 0.5 mg/dL is considered normal.The difference between groups is statistically significant (P=0.02)
Figure 2. Comparison of duration of hospitalization in children with Mycoplasma pneumoniae-associated RIME stratified by Neutrophil:Lymphocyte Ratios
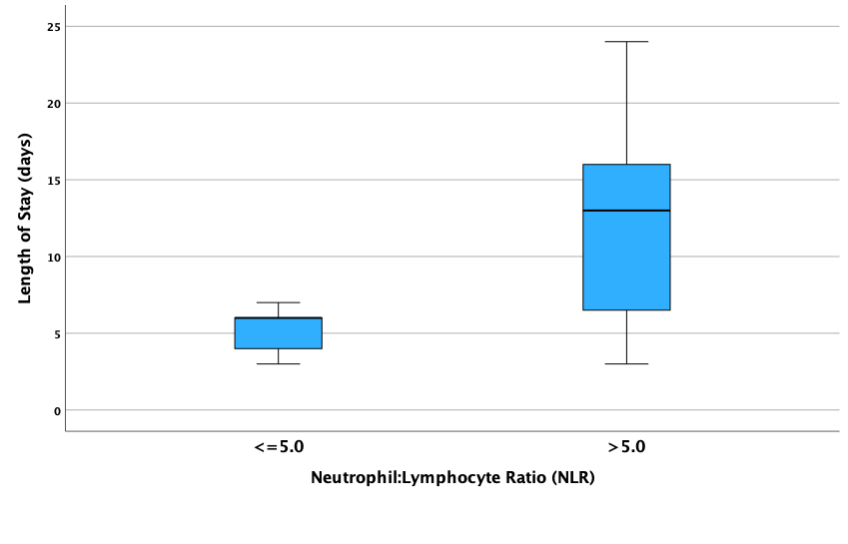 The difference between groups is statistically significant (P=0.01)
The difference between groups is statistically significant (P=0.01)
