Cardiology 1
Session: Cardiology 1
135 - Contrast Enhanced Three-Dimensional Echocardiographic Quantification of Right Ventricular Volumes Compared to Cardiac Magnetic Resonance Imaging In Repaired Congenital Heart Disease
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 135.4471
Christiane Mhanna, Nemours Children's Hospital, Wilmington, DE, United States; Ligia Han, Nemours Children's Hospital, Wilmington, DE, United States; Mya Carney, Nemours Children’s Health, Media, PA, United States; Mark Cartoski, NemoursAlfred I. duPont Hospital for Children, Wilmington, DE, United States; Shubhika Srivastava, NemoursAlfred I. duPont Hospital for Children, Wilmington, DE, United States; Praveen Mehrotra, Thomas Jefferson University Hospital, Philadelphia, PA, United States; Carol Prospero, Nemours Children's Hospital, Wilmington, DE, United States; varsha Zadokar, Nemours Children’s Hospital, Wilmington, DE, United States; Shannon N. Nees, Nemours Children's Hospital, Wilmington, DE, United States; Matthew J. Campbell, Baylor College of Medicine, Houston, TX, United States

Christiane Mhanna, D.O.
Pediatric Cardiology Fellow
Nemours Children's Hospital
Wilmington, Delaware, United States
Presenting Author(s)
Background: Due to the complex geometry of the right ventricle (RV), cardiac magnetic resonance imaging (CMR) is the reference standard for assessing RV size and function. Ultrasound enhancing agents have improved 3D echocardiogram (3DE)-derived estimates of RV size and function in adult patients. Combining ultrasound enhancing agents and 3DE assessment of the RV has not yet been applied to repaired congenital heart disease (CHD).
Objective: The objective was to assess RV size and function in patients with repaired CHD with residual pulmonary regurgitation by comparing noncontrast and contrast enhanced 3DE with semi-automated RV analysis to CMR derived values.
Design/Methods: A single center, prospective study using 3DE with semi-automated RV analysis software with and without administration of an ultrasound enhancing agent (sulfur hexafluoride lipid-type A microspheres) was performed. Patients ≥ 11 years old with repaired CHD and residual pulmonary insufficiency were eligible. Immediately following clinically indicated CMR, enrolled patients underwent noncontrast and contrast enhanced 3DE. RV volume and function were compared between CMR, noncontrast and contrast enhanced 3DE.
Results: Twenty-two patients (12 male; mean age 19.8 years) were enrolled. Two were excluded due to imaging and technical limitations. In total, 19 noncontrast and 15 contrast 3DEs were sufficient for analysis based on image quality. Noncontrast 3DE RV end diastolic volume (EDV) demonstrated good correlation with CMR (R2=0.75, p<.001, mean % difference 11.9%, IQR 3.9%-19.3%). Contrast enhanced 3DE RVEDV demonstrated moderate correlation with CMR (R2=0.58, p=.001, mean % difference 19.3%, IQR 7.7%-29.8%) (Figure 1). Mean RVEDV estimate for noncontrast and contrast enhanced 3DE underestimated CMR derived RVEDV, but this was not uniform (Figure 2). Noncontrast 3DE showed poor correlation with ejection fraction (R2=0.25, p=.03) and contrast 3DE was not correlated with CMR derived ejection fraction. There were no adverse advents.
Conclusion(s): Noncontrast 3DE showed good correlation with CMR derived RVEDV and outperformed contrast enhanced 3DE. There were still significant outliers, likely due to challenges in imaging outflow tracts. Challenges with contrast imaging included a significant decrease in frame rate with contrast settings and software that was not designed for use with ultrasound enhancing agents. 3DE is useful for estimating RV size, but limitations persist in patients after repaired CHD.
Figure 1.
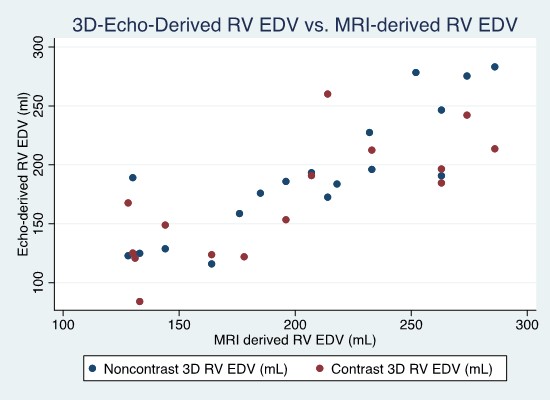 Scatter plot of noncontrast and contrast 3DE derived RVEDV versus CMR derived RVEDV.
Scatter plot of noncontrast and contrast 3DE derived RVEDV versus CMR derived RVEDV. Figure 2.
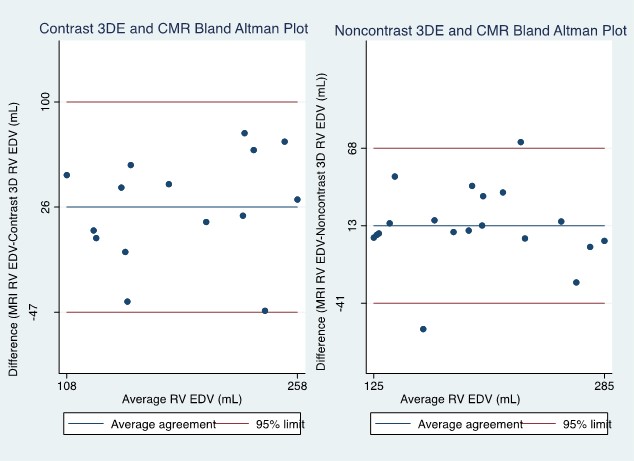 Bland Altman Plot of contrast 3DE, noncontrast 3DE and CMR derived RVEDV.
Bland Altman Plot of contrast 3DE, noncontrast 3DE and CMR derived RVEDV. 
