Medical Education 1: Curricular innovations and assessment 1
Session: Medical Education 1: Curricular innovations and assessment 1
485 - Development and Evaluation of a Novel Guided Resident Educational Debrief Tool for Critical Events in the Neonatal Intensive Care Unit
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 485.4461
Kelsey Kirkman, Baylor College of Medicine, Houston, TX, United States; Shweta Parmekar, Baylor College of Medicine, Houston, TX, United States; Stephanie Hale, Baylor College of Medicine, Pearland, TX, United States; Melissa M.. Carbajal, Baylor College of Medicine, Houston, TX, United States
Kelsey Kirkman, MD (she/her/hers)
Neonatology Fellow
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: Despite experiencing multiple resuscitation events in the neonatal intensive care unit (NICU) and throughout other units, pediatric residents at our institution have expressed that they participate in debriefs less than 50% of the time, with only some feeling satisfied with debriefing. Studies have shown that debriefing after critical events can improve clinician knowledge and skill acquisition. While there are validated debrief tools for simulation in the literature, there are little to no published debrief tools focusing on medical education for in situ events. Can a new resident educational debrief tool increase the frequency of debriefs, the satisfaction of debriefs, and improve resident medical knowledge following critical patient incidents in the NICU?
Objective: (1) To develop a novel educational debrief tool for resident physicians to use after acute critical events. (2) To evaluate the efficacy of this debrief tool in the NICU
Design/Methods: We applied several educational theories into our theoretical framework for the development of our tool. Incorporating results from a needs assessment, and using a Delphi consensus model with expert input, the tool was finalized. To evaluate the tool’s implementation in the NICU, residents filled out pre- and post-rotation surveys about their perspectives on debriefing and the use of this tool. Chi-square analysis was done on the survey results. After each rotation, exit interviews were conducted with the residents to better understand their experiences with the tool.
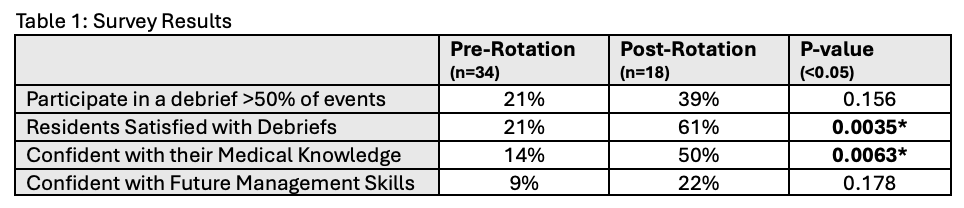
Results: During the study period, 11 residents used the tool during their NICU rotation and 8 critical events were debriefed with the tool. Based on survey responses, all who used the tool were satisfied with the debrief and all felt they were able to learn something from the discussion. Chi-square analysis was completed, which showed a significant increase in resident satisfaction and confidence in their medical knowledge (Table 1). Overall impressions from the interviews also confirmed that they were more satisfied with this structured educational debrief tool.
Conclusion(s): In our study population, having a standardized tool focused on resident medical education has improved resident satisfaction with debriefs and led to improvement in medical knowledge. While there was no significant improvement in the frequency of debriefs occurring with our tool, we believe this could be limited by the small sample size, and observing over a longer data collection period might be helpful. Future directions include doing thematic analysis on the interviews to further assess residents’ debriefing experiences.
Figure 1. Finalized Debrief Tool
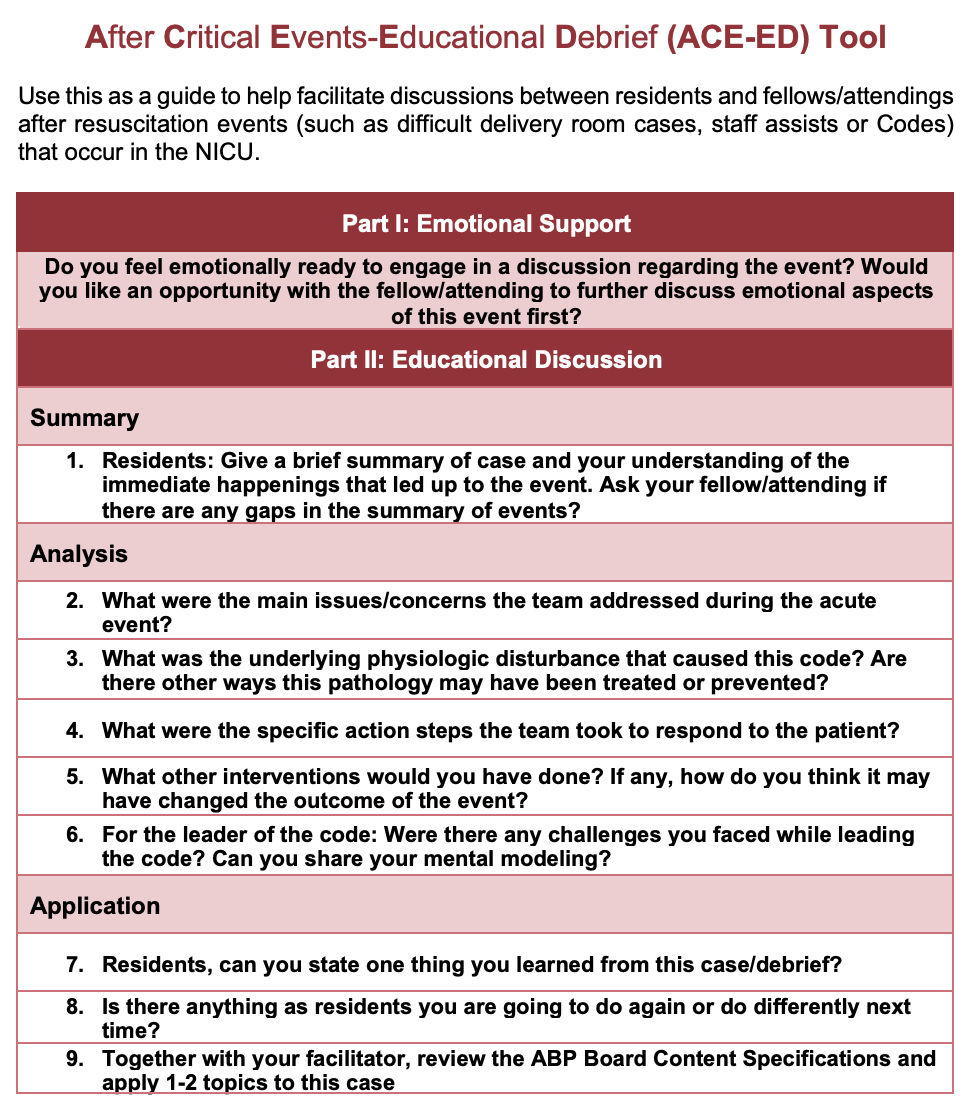 After Critical Events- Educational Debrief (ACE-ED) Tool
After Critical Events- Educational Debrief (ACE-ED) Tool Table 1. Survey Results