General Pediatrics 1
Session: General Pediatrics 1
692 - Effect of an EHR prompt and patient-centered resource toolkit on quality of dietary history documentation by providers in a public hospital primary care pediatric clinic
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 692.4824
Nicole Werner, Hassenfeld Children's Hospital at NYU Langone, New York, NY, United States; Serena Chen, NYU Langone Health, New York, NY, United States; Abigail L. Nita, Indiana University School of Medicine, Fort Wayne, IN, United States; Olivia Lee, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; Nikita Nagpal, New York University Grossman School of Medicine, New York, NY, United States; Carol Duh-Leong, Hassenfeld Children's Hospital at NYU Langone, New York, NY, United States; Stephanie Quintero Chacon, NYU Langone Health, East Elmhurst, NY, United States; Robin Ortiz, New York University Grossman School of Medicine, New York, NY, United States

Nicole Werner (she/her/hers)
Medical Student
Hassenfeld Children's Hospital at NYU Langone
New York, New York, United States
Presenting Author(s)
Background: Many children in the U.S. don't consistently eat fruits and vegetables, despite the critical role of early nutrition in growth, development, and overall health. Although pediatric guidelines emphasize the importance of dietary counseling, there is limited research on standardized methods for assessing dietary history, counseling, and documentation in routine well-child encounters.
Objective: To evaluate the effect of a two-step strategy on frequency and quality of dietary history documentation including: 1) an electronic health record (EHR) dietary documentation template and subsequently, 2) the option to provide a tangible healthy habits toolkit to patients.
Design/Methods: EHR templates for well child visits at age 3-11 years at a public hospital pediatric primary care clinic were updated from a general open diet history prompt to quantify, 1) the daily fruit and vegetable serving intake for the child and, 2) the accompanying caregiver. After a 10-week period, toolkits containing caregiver-child supports for healthy habits (workbook, measuring cups, water bottle, Healthbuck dollars for farmers market use) were available for children with < 2 daily servings. Providers were notified of each strategy by verbal and email announcements.
Retrospective chart analysis of 600 charts was done to quantify the frequency of documentation. Using a content saturation approach, 120 randomly selected charts, half prior to and half succeeding the new EHR template, were analyzed qualitatively for dietary history content, guided by the AAP’s healthy habits questionnaire.
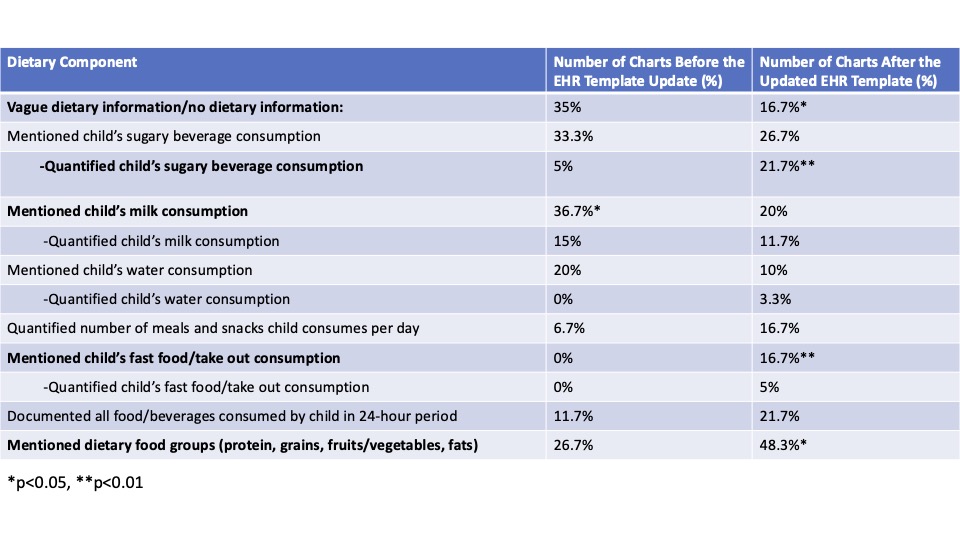
Results: Prior to any intervention, 0 of the 60 analyzed charts documented daily servings of fruits and vegetables. Following introduction of the EHR template but preceding toolkit introduction, 36.1% of charts recorded daily fruit/vegetable servings. Following introduction of the toolkits 61.4% documented fruit/vegetable intake (Table 1). Qualitative analysis demonstrated a decrease in missing dietary documentation or vague dietary documentation, such as “varied diet” or “most food groups” (Table 2).
Conclusion(s): Implementing an EHR-based prompt to quantify dietary intake has the potential to enhance screening for healthy dietary intake. Adding an external, tangible reminder outside of the EHR may augment its effectiveness. Further, the observed improvement in dietary history documentation without modification to clinic workflow suggests these approaches are feasible in primary care settings. Future studies aim to evaluate the impact of these approaches on the quality of the clinician-patient interactions and, ultimately, on patient-centered outcomes.
Table 1: Comparing frequency of chart documentation before and after intervention implementation
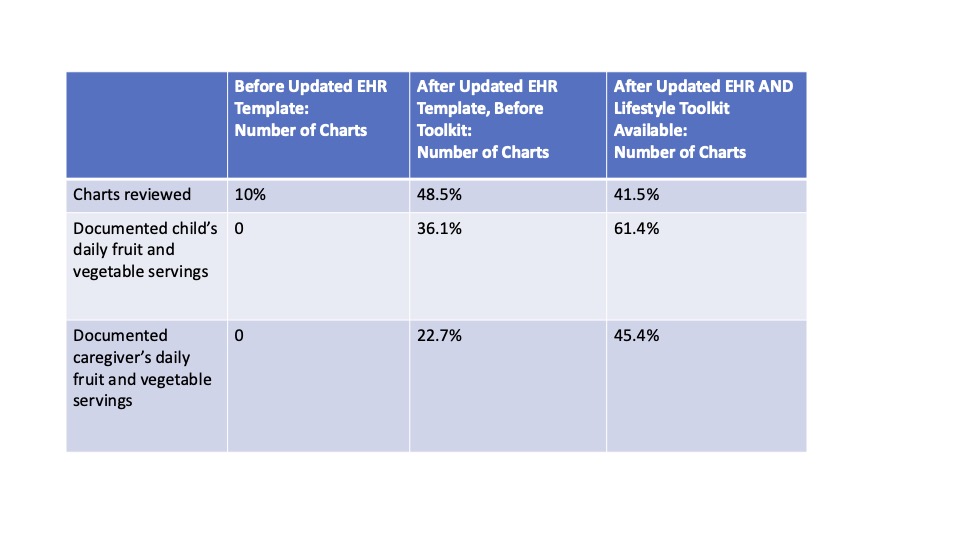
Figure 1: Schematic of experimental design
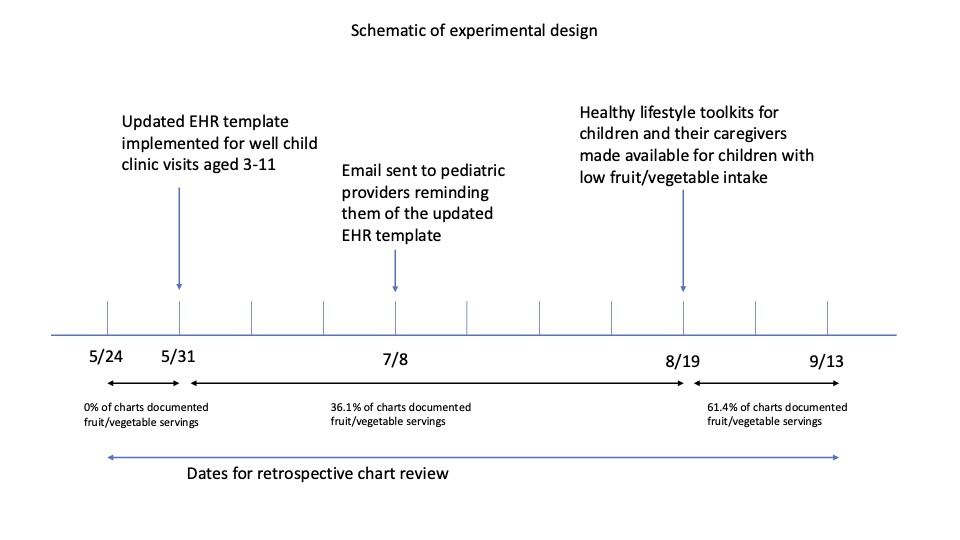
Table 2: Qualitative analysis of charts' dietary history content, before and after intervention