Neonatal Quality Improvement 1
Session: Neonatal Quality Improvement 1
059 - Improving First Attempt Neonatal Intubation Success: A Quality Improvement Initiative
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 59.5176
Mohamed W. Mohamed, Sanford Children's Hospital - Fargo, Fargo, ND, United States; Traci Williams, Sanford Children's Hospital - Fargo, Fargo, ND, United States; Kimberly J. Haug, Sanford Children's Hospital - Fargo, Fargo, ND, United States; Tara Heidrich, Sanford Children's Hospital - Fargo, Moorhead, MN, United States; May Kamleh, ICON Clinical Outcomes, La Grange, IL, United States

Mohamed W. Mohamed, MD (he/him/his)
Neonatologist
Sanford Children's Hospital - Fargo
Fargo, North Dakota, United States
Presenting Author(s)
Background: Neonatal intubation in the Neonatal Intensive Care Unit (NICU) is a procedure often necessary for preterm or critically ill infants. However,multiple intubation attempts have been associated with adverse events such as intraventricular hemorrhage, pneumothorax, direct airway trauma, and cardiorespiratory arrest. Pre-intervention data from Sanford Health's NICU showed low first-attempt successful intubation (FASI) rate which highlighted the need for standardized, evidence-based protocols to increase success and decrease adverse outcomes related to multiple intubation attempts.
Objective: The objective of this quality improvement initiative was to increase the FASI rate through the implementation of standardized intubation procedures, including the use of video laryngoscopy (VL) and premedication protocol
Design/Methods: This initiative was implemented through two Plan-Do-Study-Act (PDSA) cycles over four years. During PDSA Cycle 1 (2020-2022), NICU staff received comprehensive re-education on the use of VL. A standardized intubation protocol was developed alongside a detailed checklist to ensure procedural adherence and consistency across all intubations. In PDSA Cycle 2 (2022-2024), the focus shifted to refining premedication protocol. Premedication bundles were tailored to align with the gestational and postnatal age of the infants to optimize sedation. Continuous staff education and feedback were sought throughout both cycles to reinforce best practices and drive improvements.
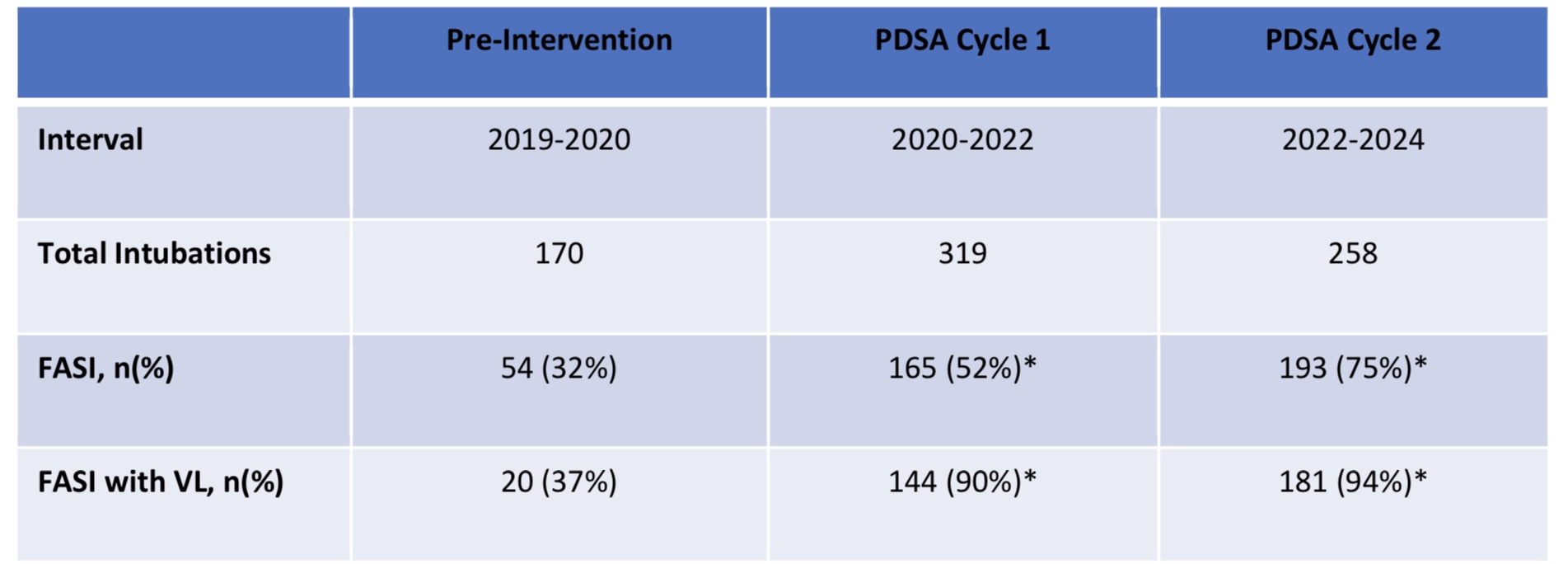
Results: Pre-intervention, the FASI rate was 32%, with FASI using VL at 37%. Following PDSA Cycle 1, significant improvements in the overall FASI rate (52%, p< 0.001) and FASI using VL-specific intubation success (905, p< 0.001) were shown as demonstrated in Table 1. These early results validated the initial changes made to the procedure and encouraged further refinement during the next phase. During PDSA Cycle 2, after revising the premedication protocols, the overall FASI rate increased further to 75% (p < 0.001), with VL-specific success rates climbing to 94% (p < 0.001). The cumulative effect of these interventions across both cycles represents a 43% overall improvement in the FASI rate, from 32% pre-intervention to 75% by the end of the second cycle. Similarly, the success rate for intubations using VL rose from 37% to 94%, highlighting the substantial role of VL in improving intubation outcomes.
Conclusion(s): The Implementation of VL and a standardized premedication protocol significantly improved FASI rates in the NICU, highlighting an important quality improvement initiative for minimizing adverse outcomes.
Table 1: FASI rate before and after intervention. Post intervention divided into two PDSA cycles. *Differences in proportions are statistically significant.t p<0.001 using Z-test of proportions.
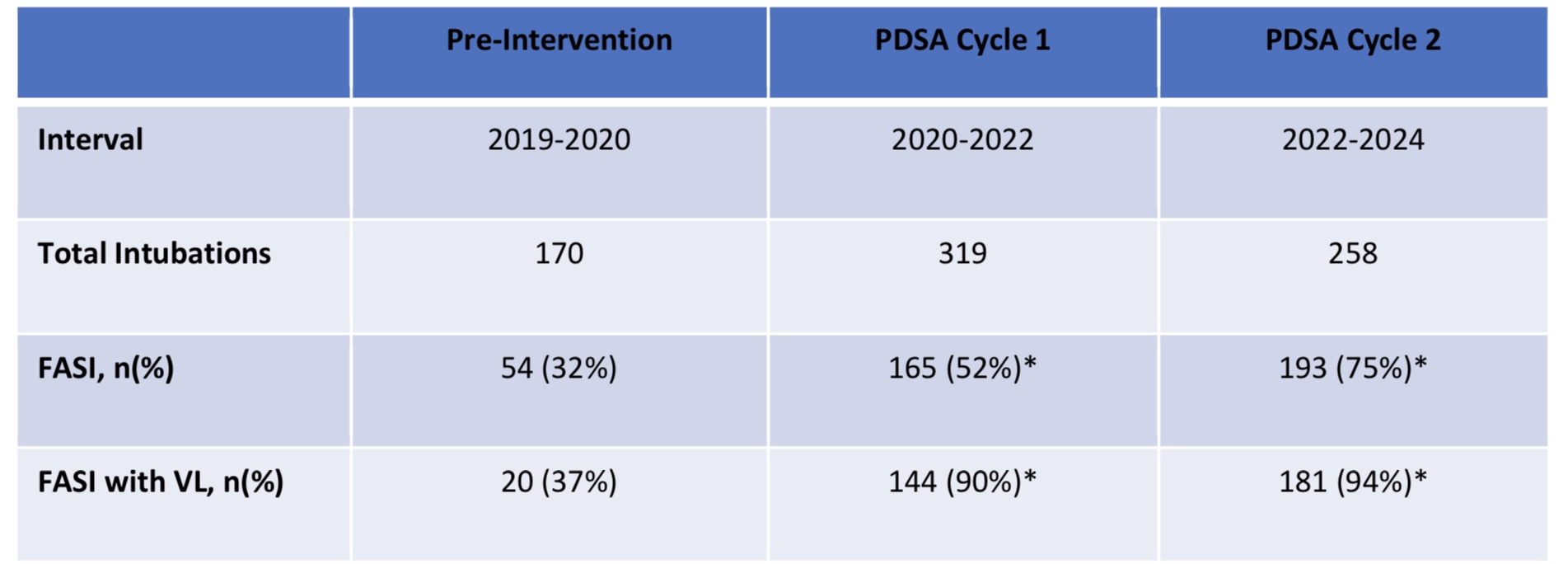
Table 1: FASI rate before and after intervention. Post intervention divided into two PDSA cycles. *Differences in proportions are statistically significant.t p<0.001 using Z-test of proportions.