Quality Improvement/Patient Safety 1
Session: Quality Improvement/Patient Safety 1
005 - Implementation of an EHR-Based PICU Rounding Checklist
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 5.5171
Laura G. Amar-Dolan, Tufts University School of Medicine, South Portland, ME, United States; Jessica Miller, The Barbara Bush Children's Hospital at Maine Medical Center, Falmouth, ME, United States; Allison Haynes, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States; Jillian Gregory, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States
- LA
Laura G. Amar-Dolan, MD (she/her/hers)
Assistant Professor of Pediatrics
Tufts University School of Medicine
South Portland, Maine, United States
Presenting Author(s)
Background: Rounding checklists have been implemented in many pediatric critical care units to support communication and adherence to evidence-based practice. A paper rounding checklist introduced to the PICU in 2022 was used infrequently.
Objective: This quality improvement project was undertaken in an eight-bed PICU at an academic tertiary care center staffed with residents and pediatric intensivists. Our checklist elements include endotracheal tube position, line necessity, diagnostic and infusion orders, prophylaxis, fluid goals, nephrotoxic medications, delirium screening, sedation, weight, skin concerns, timely transfer/discharge. Our aim was to increase checklist use to 75% over one year and determine its impact on patient care, team communication, and rounding time.
Design/Methods: We used a PDSA QI methodology with input from the multidisciplinary ICU team. Input was collected via surveys, quality committee meetings, and in-unit quality rounds. Perceived barriers to use of the paper checklist included inability to locate the checklist, lack of ready access to relevant data, and a lack of attending physician leadership on checklist use. We developed an EHR embedded rounding checklist and PICU-specific clinical overview tab. Educational interventions were undertaken with attendings, residents, and nurses to increase checklist use. The checklist was revised to include additional decision support and branching logic. Checklist completion, plan changes, and time spent on the checklist were monitored by direct observation. A survey was sent to the multidisciplinary ICU team before and after implementation of the EHR based checklist. Checklist completion data was analyzed using SPC charts. Survey responses were analyzed using the Cochran Armitage Test.
Results: Prior to the EHR version the checklist completion rate was 15%. After implementation we noted a centerline shift to 67%. When reviewed, the checklist led to one or more changes in the care plan 18% of the time. It took an average of 1 minute to complete per patient. After introduction of the EHR based checklist, more respondents agreed or strongly agreed that the survey is used (20.5% to 81.4%, p<.001) and is easy to use (61.3% to 88.9%, p=.003).
Conclusion(s): Implementation of an EHR based checklist developed with input from our multidisciplinary ICU team has increased checklist use. The checklist is perceived as easy to use and has contributed to changes in patient care. Ongoing work is needed to determine the impact on patient outcomes. Barriers to sustained change include staff turnover and ensuring all team members are present for checklist review.
Rounding Checklist Completion
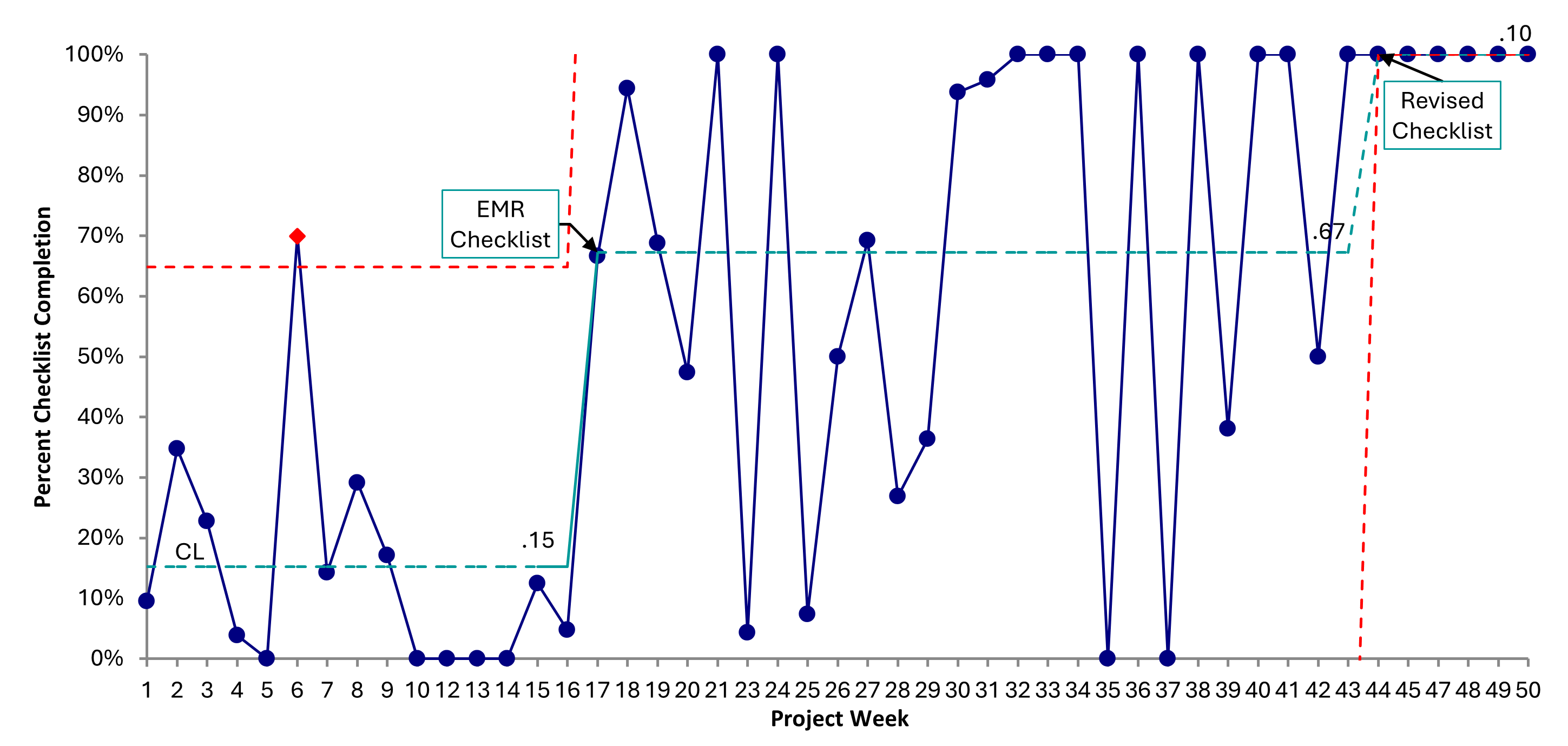 P-chart showing rates of rounding checklist completion by project week. Process changes are annotated.
P-chart showing rates of rounding checklist completion by project week. Process changes are annotated. Changes to Care Plan
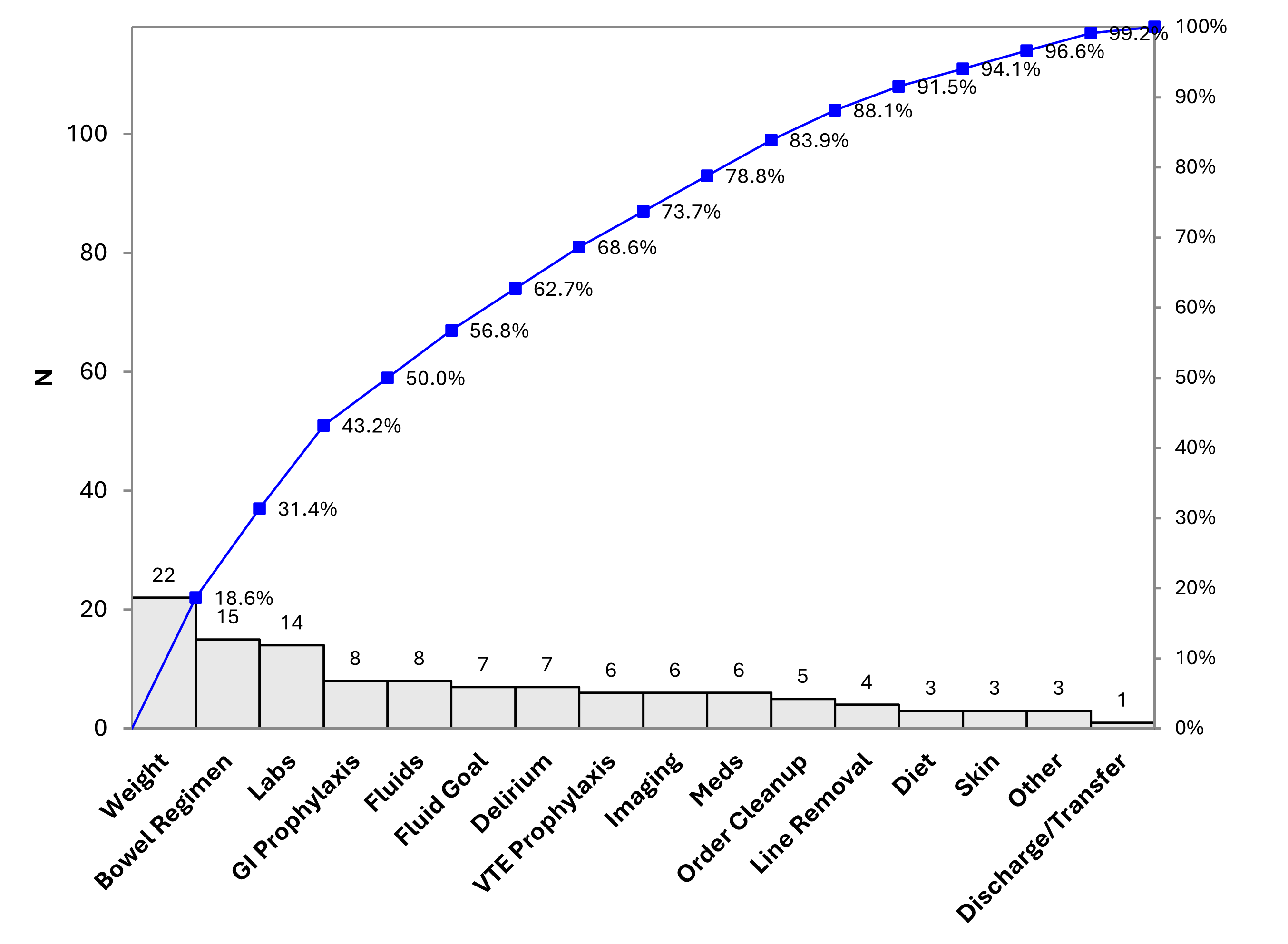 Pareto chart of care plan changes made during review of rounding checklist.
Pareto chart of care plan changes made during review of rounding checklist. Rounding Checklist Completion
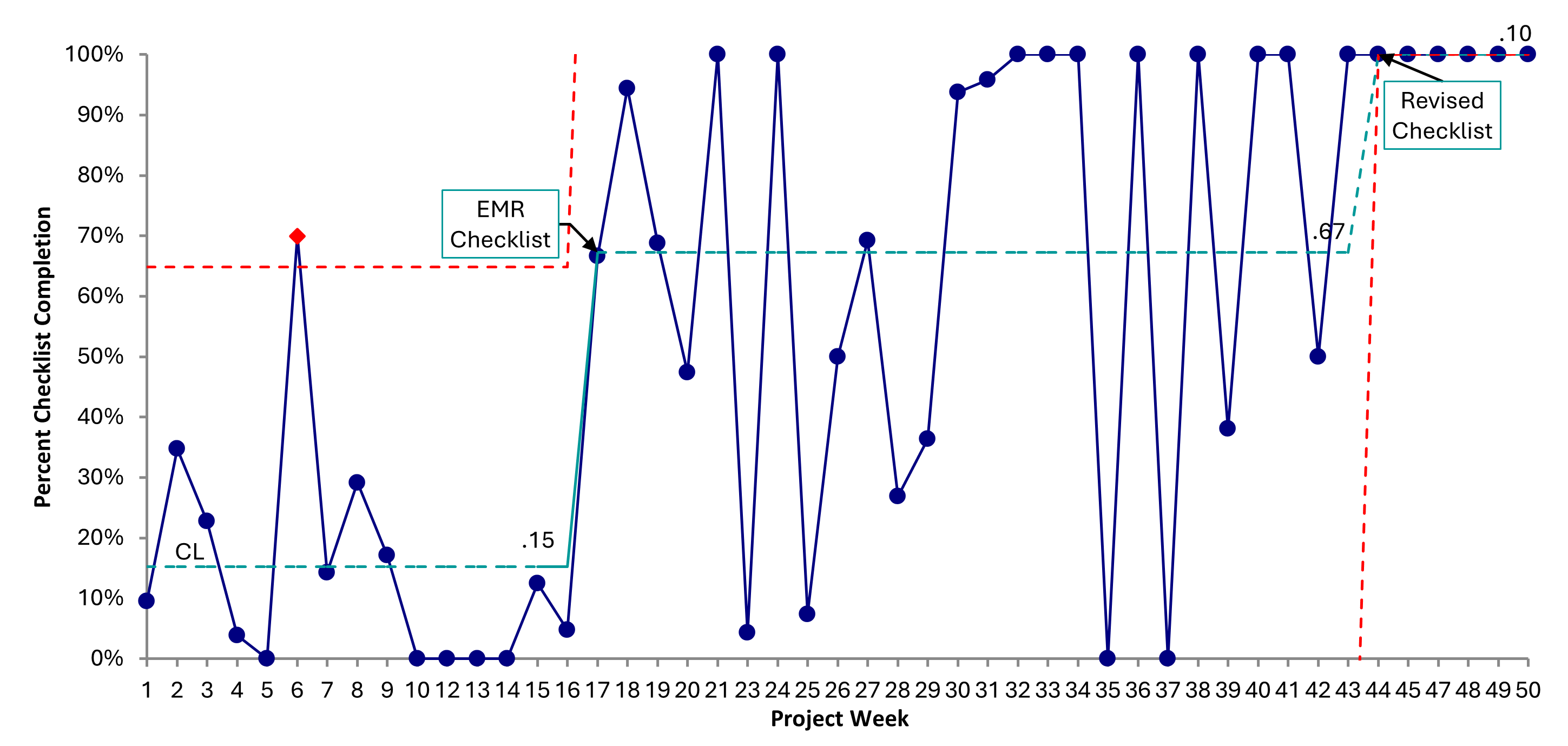 P-chart showing rates of rounding checklist completion by project week. Process changes are annotated.
P-chart showing rates of rounding checklist completion by project week. Process changes are annotated. Changes to Care Plan
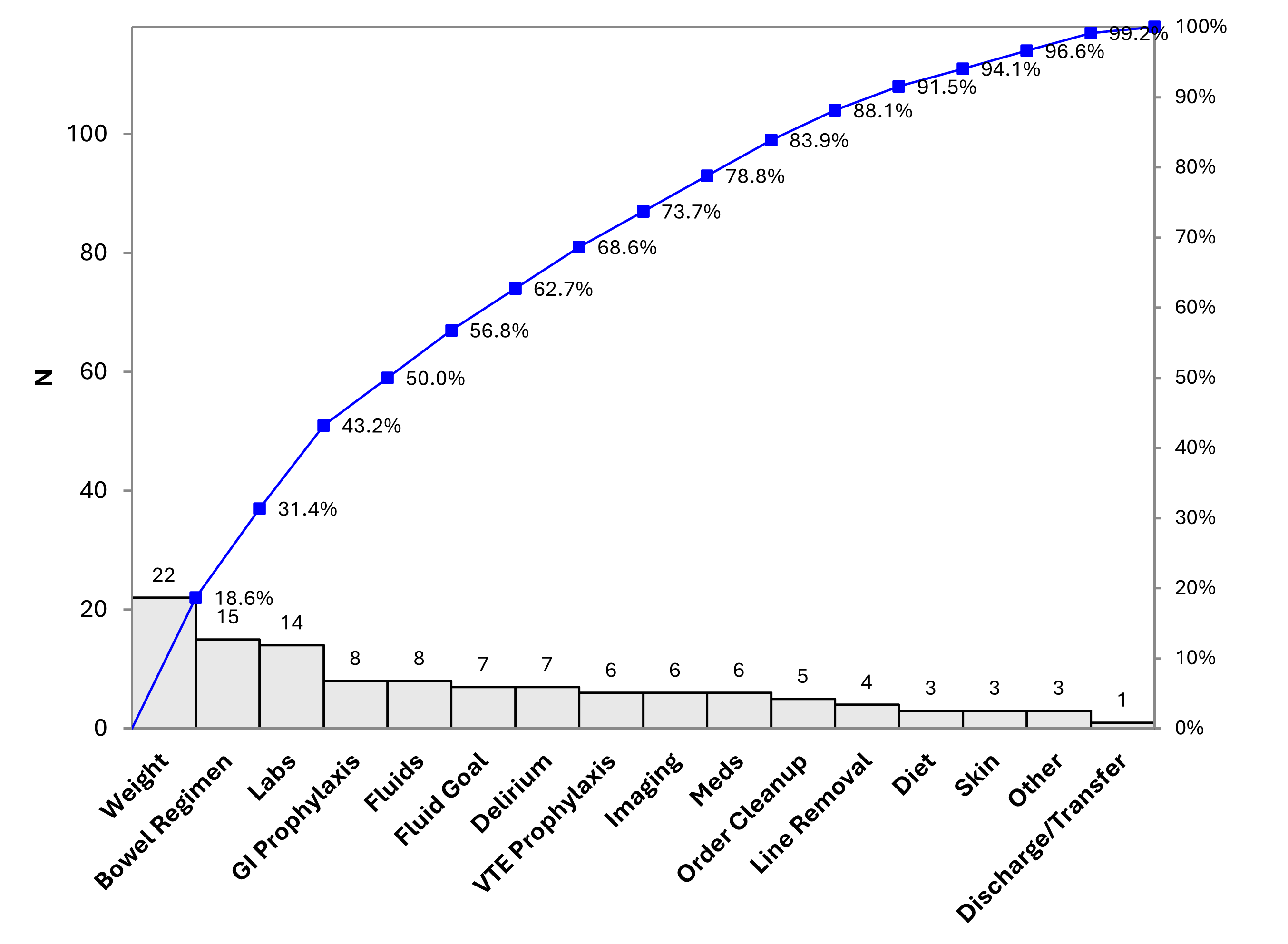 Pareto chart of care plan changes made during review of rounding checklist.
Pareto chart of care plan changes made during review of rounding checklist. 

