Neo-Perinatal Health Care Delivery: Practices and Procedures 1
Session: Neo-Perinatal Health Care Delivery: Practices and Procedures 1
457 - Improving outcomes of periviable births via an enhanced prediction tool
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 457.5164
Henry C. Lee, University of California, San Diego School of Medicine, La Jolla, CA, United States; Deirdre Judith. Lyell, Lucile Packard Children's Hospital Stanford, Stanford, CA, United States; Xiao Xu, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Jeff Gould, Stanford University School of Medicine, Berkely, CA, United States; Kristen E. Schaffer, University of California, San Diego School of Medicine, La Jolla, CA, United States; Tianyao Lu, Stanford University CPQCC, alamo, CA, United States; Emily Silliman, University of California, San Diego School of Medicine, La Jolla, CA, United States; Susan R. Hintz, Stanford University School of Medicine, Palo Alto, CA, United States
Henry Lee, MD (he/him/his)
Professor
University of California San Diego
La Jolla, California, United States
Presenting Author(s)
Background: For infants born extremely preterm, the hope of survival must be weighed against the trauma that infants and families may undergo in efforts to resuscitate and care for an infant that may ultimately have a very short life or severe life-long disability. Clinicians often lack the ability to provide the most accurate and up-to-date information to families during counseling. Current prediction models often rely on older data, are not tailored to birth institution, or use limited information to make predictions.
Objective: To assess usage patterns of a new prognostic prediction tool for extremely preterm birth based on contemporary data from the California Perinatal Quality Care Collaborative (CPQCC) and implemented across California hospitals.
Design/Methods: We developed a prognostic prediction model for extremely preterm birth using CPQCC data on infants born at 22+0 to 25+6 weeks gestation from 2018 to 2022 (n=3998), excluding those with congenital abnormalities or without active resuscitation. The final model included the following maternal and infant risk factors: gestational age (weeks and days), intrauterine growth restriction (IUGR), multiple birth, infant sex, and antenatal steroid administration. Birth hospital was included as a random effect to allow for hospital-specific prediction. A web-based tool allows users to input pregnancy risk factors and generate corresponding estimates for overall survival and survival without major morbidity, defined as the absence of death during birth hospitalization, chronic lung disease, severe peri-intraventricular hemorrhage, nosocomial infection, necrotizing enterocolitis, severe retinopathy of prematurity, and cystic periventricular leukomalacia. The tool was implemented across 116 CPQCC hospitals between August 2023 and September 2024 using a stepped wedge design. Neonatologists, obstetricians, and other clinicians were invited to use the tool.
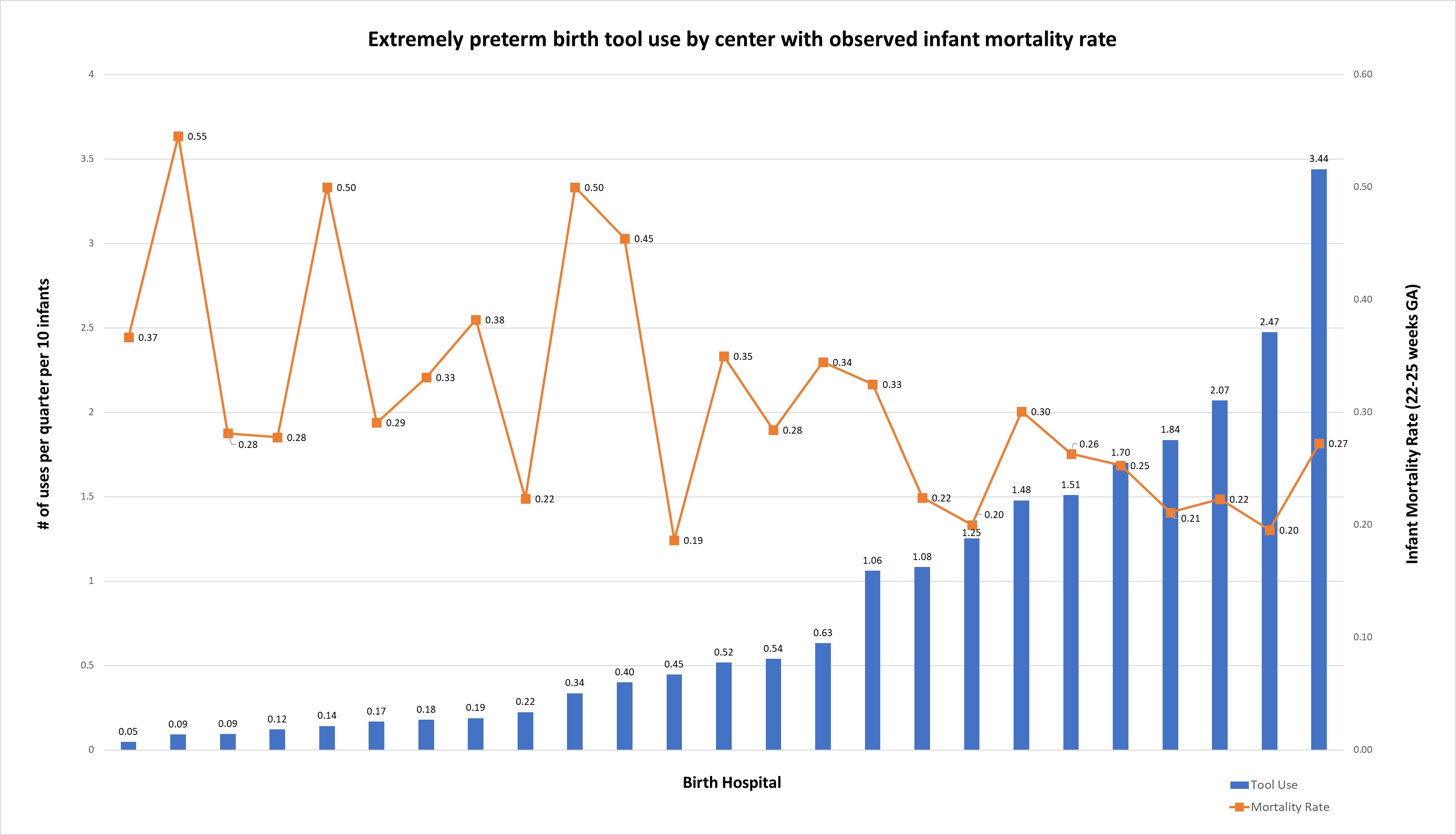
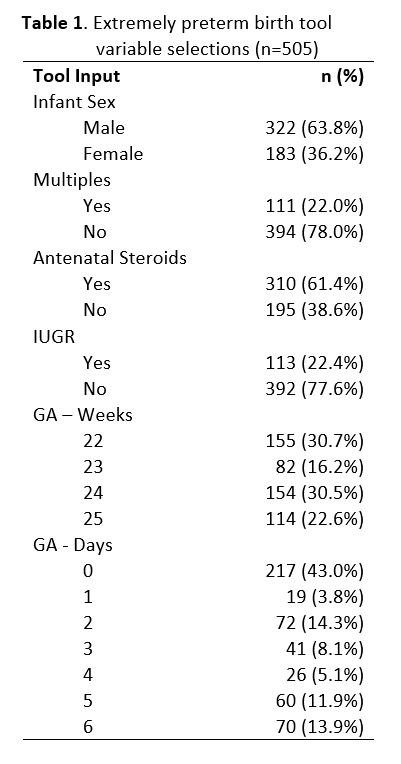
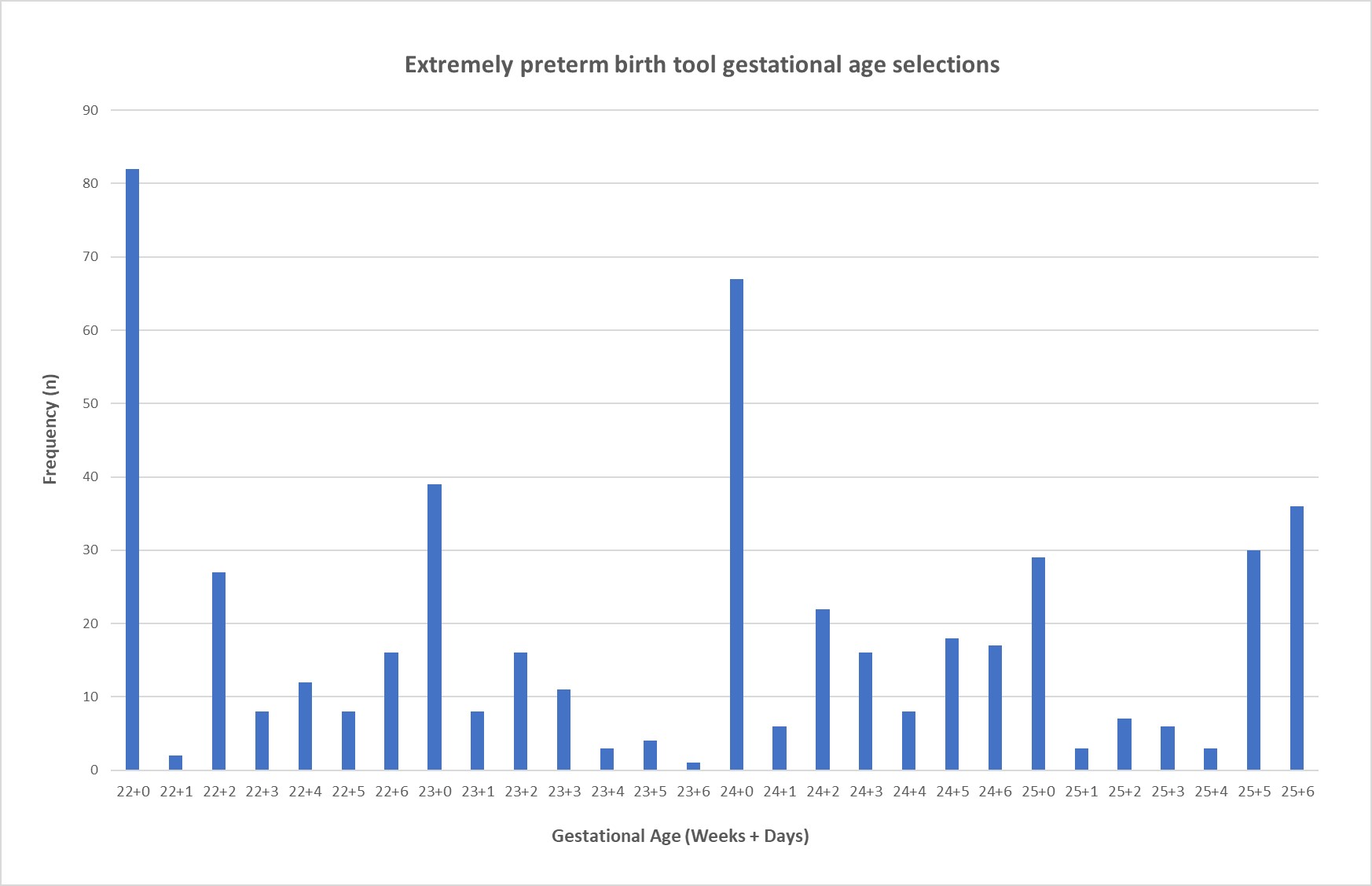
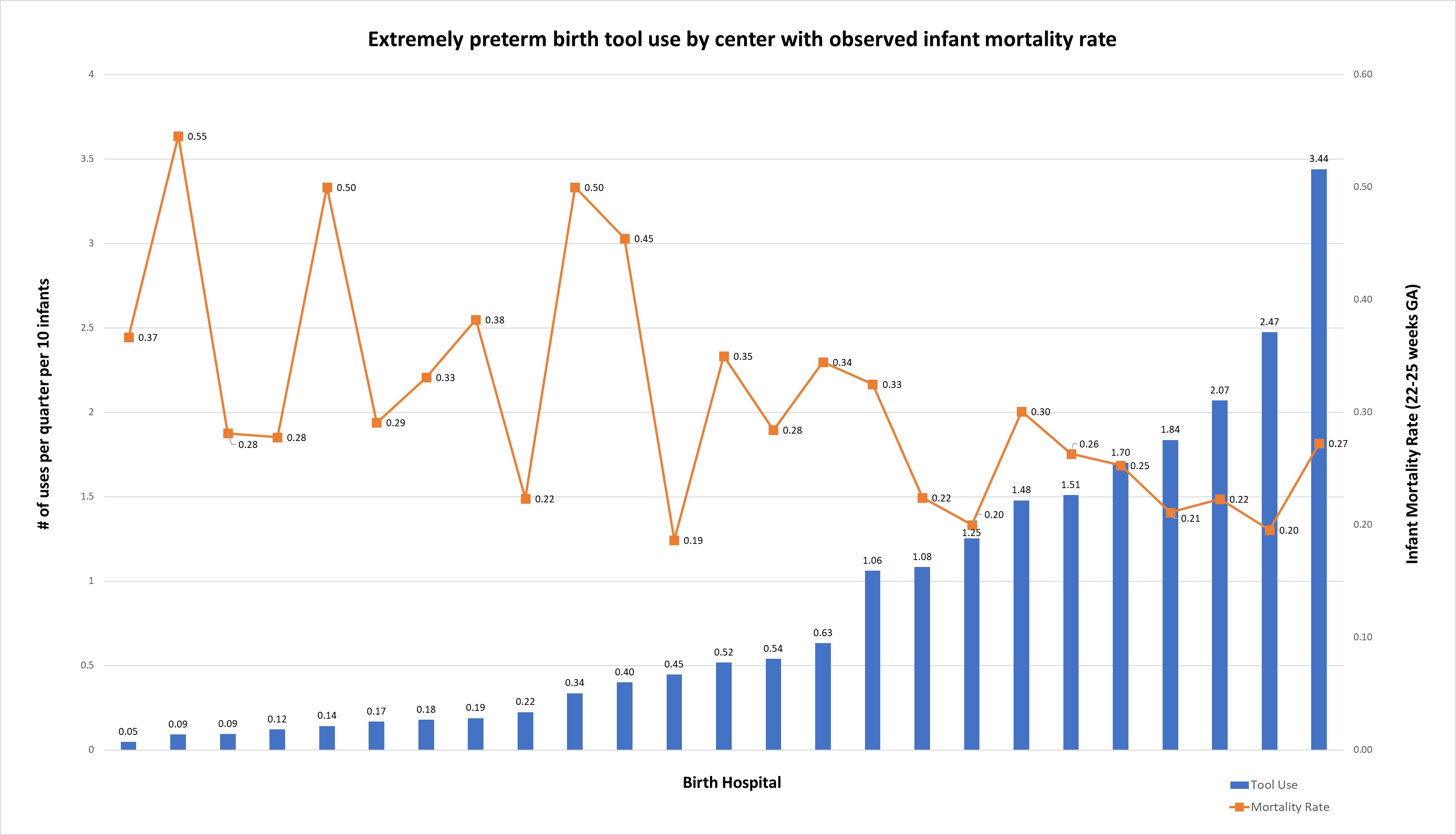
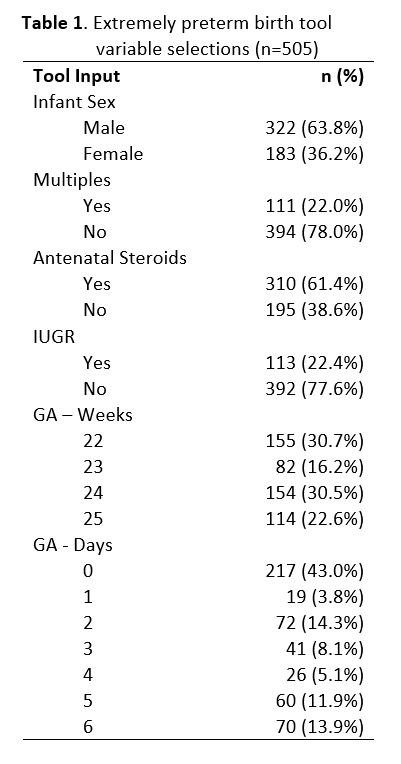
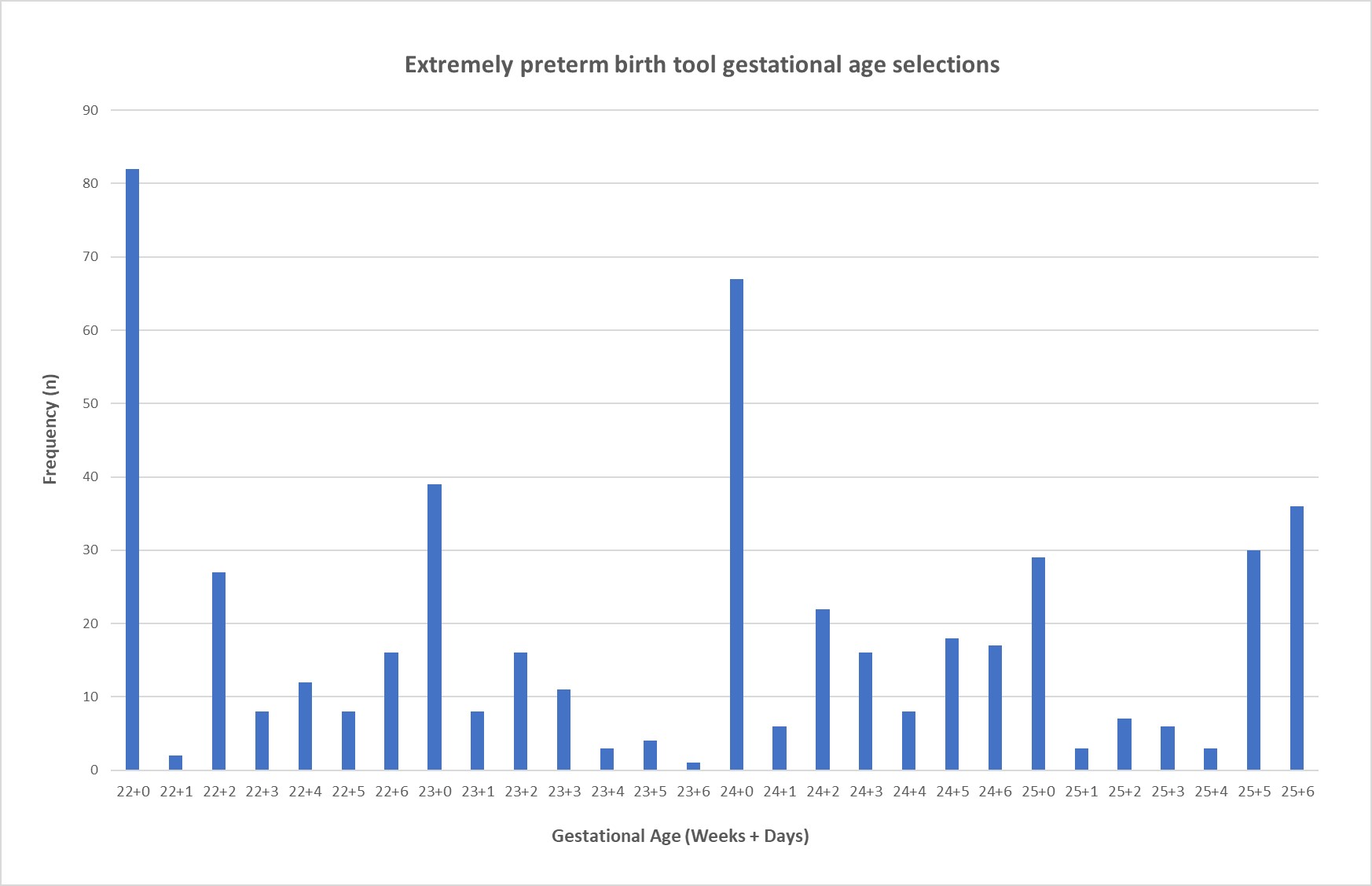
Results: Ninety-one clinicians across 60 hospitals registered to use the tool; 505 unique tool calculations were identified. The majority of birth scenarios evaluated were male (64%), singletons (78%), without IUGR (78%), and having received antenatal steroids (61%) (Table 1). The most common gestational age evaluated was 22+0, followed by 24+0 and 25+6 (Figure 1). Increased tool use by hospital was associated with lower mortality rate for infants born at 22-25 weeks gestation (Figure 2).
Conclusion(s): The results provide a preliminary understanding of utilization patterns of the new CPQCC periviability prognostic prediction tool. Further research is needed to understand tool user experience and its clinical utility.
Extremely preterm birth tool variable selections
Extremely preterm birth tool gestational age selections
Extremely preterm birth tool use by center with observed infant mortality rate
Extremely preterm birth tool variable selections
Extremely preterm birth tool gestational age selections
Extremely preterm birth tool use by center with observed infant mortality rate