Emergency Medicine 3
Session: Emergency Medicine 3
442 - Identifying a temperature threshold for bacterial infections among infants presenting to the emergency department with hypothermia: a multicenter retrospective study
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 442.5146
Jamie Holland, Medical College of Wisconsin, Milwaukee, WI, United States; Sriram Ramgopal, Ann & Robert H. Lurie Children's Hospital of Chicago, Oak Park, IL, United States; Paul L. Aronson, Yale School of Medicine, New Haven, CT, United States; Theodore heyming, CHOC Children's Hospital of Orange County, Orange, CA, United States; Naghma S. Khan, Emory University School of Medicine, ATLANTA, GA, United States; Andrea T. Cruz, Baylor College of Medicine, Houston, TX, United States; Stacey L. Ulrich, Rady Children's Hospital San Diego, san diego, CA, United States; Leslie Ann. Hueschen, Children's Mercy Hospital/ University of Missouri-Kansas City, Kansas City, MO, United States; Kelly R.. Bergmann, Children’s Minnesota, University of Minnesota Masonic Children’s Hospital, Minneapolis, MN, United States; Alexander Rogers, University of Michigan Medical School, Ann Arbor, MI, United States; Laura F. Sartori, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Alexandra Geanacopoulos, Boston Children's Hospital, Boston, MA, United States; Nathan Money, University of Utah School of Medicine, Salt Lake City, UT, United States; Amy D. Thompson, Nemours Children's Hospital, Wilmington, DE, United States; Amy Zhou, University of Texas Southwestern Medical School, Dallas, TX, United States; Paria M. Wilson, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Sofia Grigoria Athanasopoulou, Yale School of Medicine, New Haven, CT, United States; Oluwakemi Badaki-Makun, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Wendi Wendt, Medical College of Wisconsin, Milwaukee, WI, United States

Jamie Holland, MD
Pediatric Emergency Medicine Fellow
Medical College of Wisconsin
Milwaukee, Wisconsin, United States
Presenting Author(s)
Background: Young infants presenting to the emergency department (ED) with hypothermia are at risk for bacterial infections, including urinary tract infections (UTI) and invasive bacterial infections (IBI; bacteremia and/or bacterial meningitis). The temperature threshold to define hypothermia based on risk for bacterial infection in this population is poorly defined.
Objective: To determine test characteristics of temperature to guide detection of bacterial infections among infants with hypothermia presenting to the ED.
Design/Methods: We performed a cross-sectional retrospective study across 16 academic pediatric EDs from January 1, 2013 through December 31, 2022 that included infants ≤90 days old with a rectal temperature of ≤36.5°C in the ED, excluding infants with fever, indwelling devices, trauma, skin and soft tissue infections, transfer from another healthcare facility, or presentation in cardiac arrest. Our outcomes were (1) UTI and/or IBI, and (2) IBI alone. We evaluated the association between the minimum temperature obtained in the ED with the presence of each outcome. We used the area under the receiver operator characteristic curve (AUROC) to assess the discriminatory role of temperature and derived the optimal cutpoint for temperature measurement based on the Euclidean distance method.
Results: We included 45,673 infants (median age 25 days [IQR 6-52]; 52.9% male). UTI and/or IBI and IBI were identified in 340 (0.7%) and 103 (0.2%), respectively. The overall median temperature for all infants was 36.3 °C (IQR 36.1-36.4 °C), which was lower in subsets of infants with UTI and IBI (36.1 °C; IQR 35.6-36.3 °C; p< 0.001 by Wilcoxon rank-sum test) and IBI alone (35.8°C; IQR 35.0-36.2 °C; p< 0.001). Using an outcome of UTI and/or IBI, the AUROC was 0.65 (95% confidence interval [CI] 0.62-0.68; Figure 1). At an optimal cutpoint of 36.1 °C, sensitivity was 52.7% and specificity was 70.0%. When using an outcome of IBI, performance was improved (AUROC 0.74, 95% CI 0.69-0.80), with a sensitivity of 63.1% and specificity of 76.6% at an optimal temperature of 36.0 °C. All cutpoints demonstrated significant tradeoffs in performance (Table 1).
Conclusion(s): In infants with hypothermia, those with UTI and/or IBI and IBI had lower temperatures than infants without these infections. All thresholds of minimum temperature to identify a higher-risk group for bacterial infections bring limitations. Future studies should incorporate both clinical and laboratory factors to refine risk stratification of hypothermic infants with suspected bacterial infections in the ED.
Figure 1
.png) Receiver operator curve of temperature with outcomes of invasive bacterial infection (IBI) and/or urinary tract infection (UTI) and IBI.
Receiver operator curve of temperature with outcomes of invasive bacterial infection (IBI) and/or urinary tract infection (UTI) and IBI.Table 1
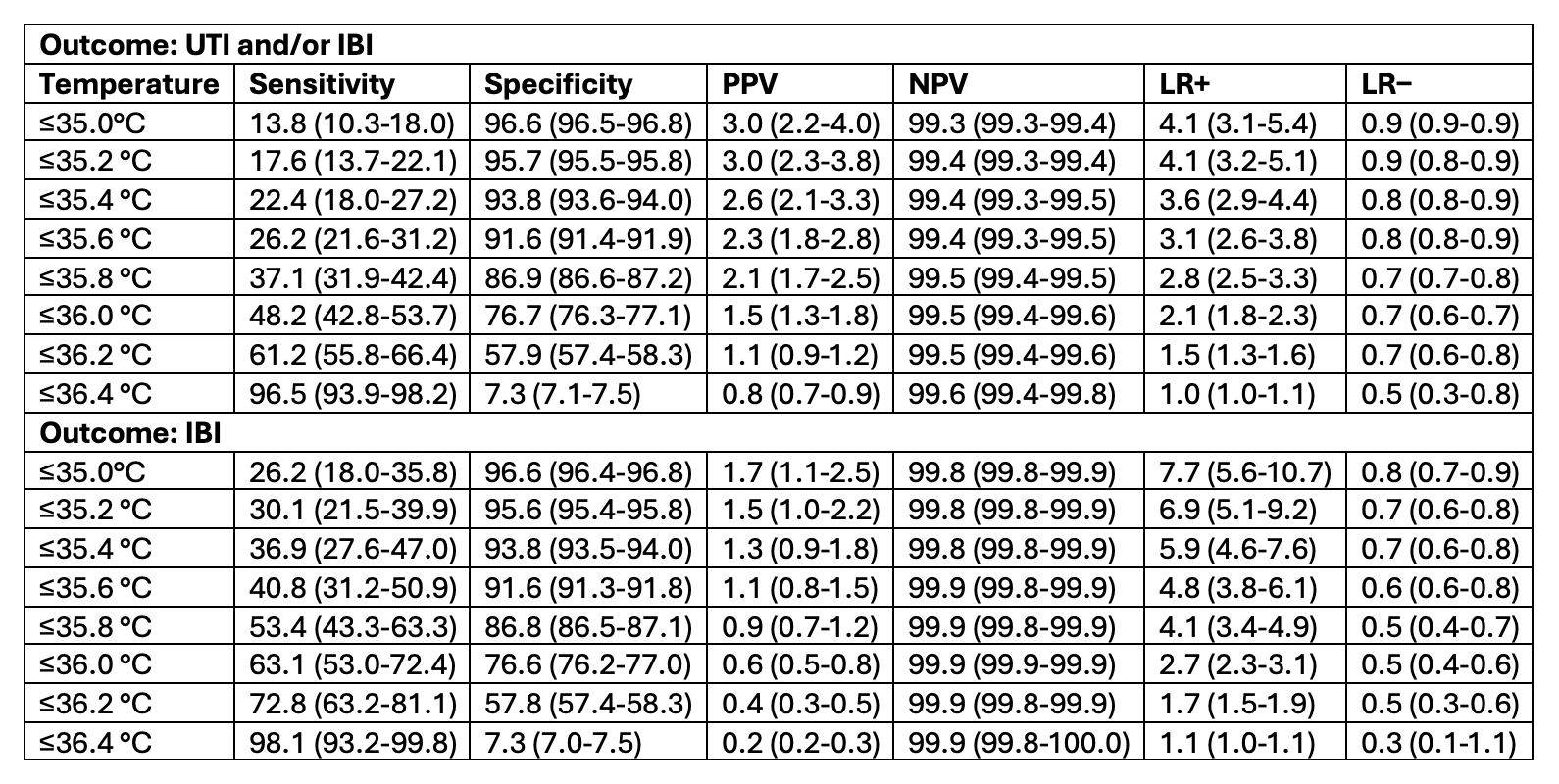 Diagnostic performance of invasive bacterial infection (IBI) and/or urinary tract infection (UTI) and IBI identification in 0.2°C increments. Numbers in parenthesis indicate 95% confidence intervals.
Diagnostic performance of invasive bacterial infection (IBI) and/or urinary tract infection (UTI) and IBI identification in 0.2°C increments. Numbers in parenthesis indicate 95% confidence intervals.Figure 1
.png) Receiver operator curve of temperature with outcomes of invasive bacterial infection (IBI) and/or urinary tract infection (UTI) and IBI.
Receiver operator curve of temperature with outcomes of invasive bacterial infection (IBI) and/or urinary tract infection (UTI) and IBI.Table 1
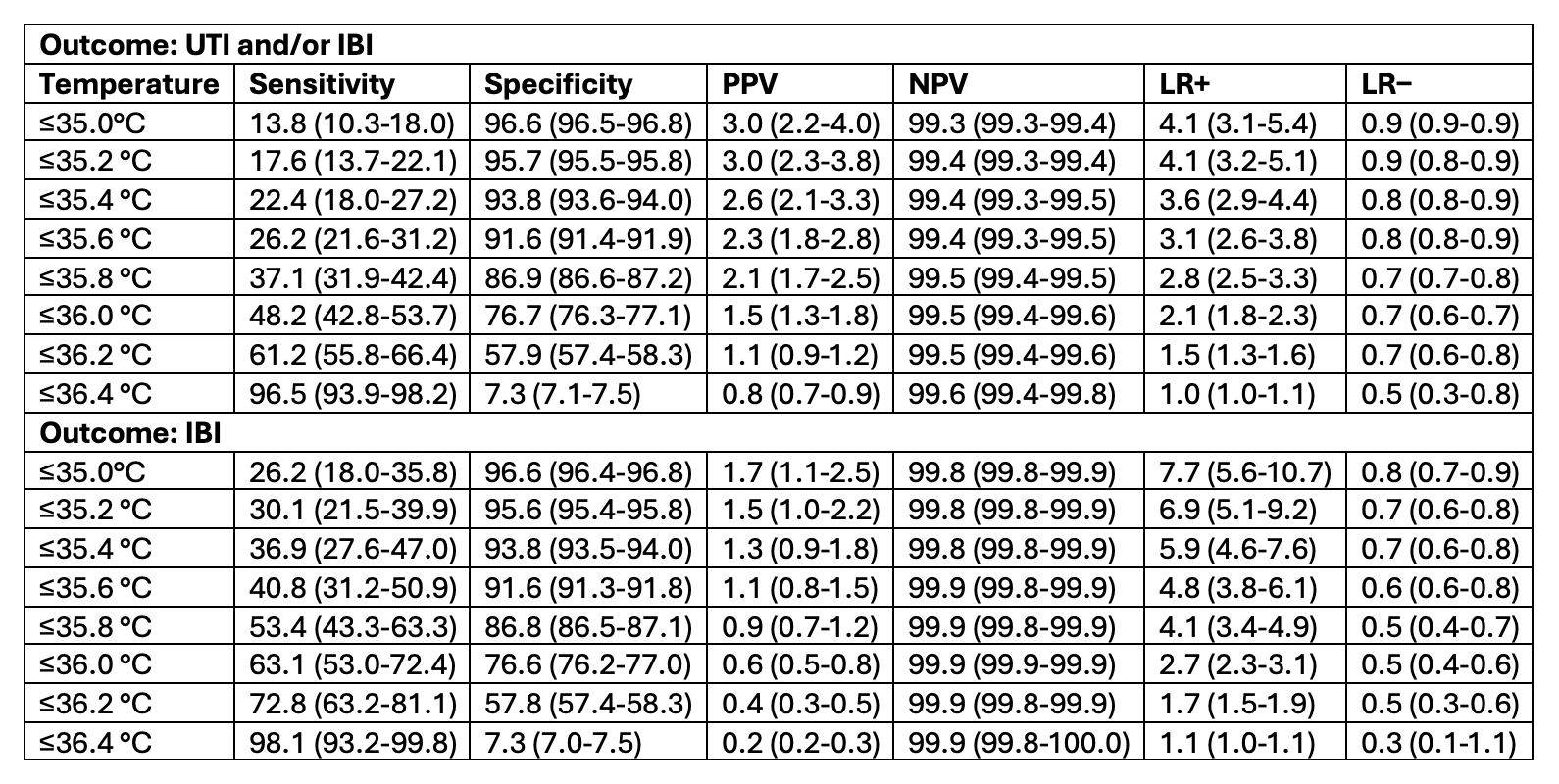 Diagnostic performance of invasive bacterial infection (IBI) and/or urinary tract infection (UTI) and IBI identification in 0.2°C increments. Numbers in parenthesis indicate 95% confidence intervals.
Diagnostic performance of invasive bacterial infection (IBI) and/or urinary tract infection (UTI) and IBI identification in 0.2°C increments. Numbers in parenthesis indicate 95% confidence intervals.
