Cardiology 2
Session: Cardiology 2
155 - Impact of Anomalous Pulmonary Venous Connections on Functional Single Ventricle Outcomes
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 155.5132
Alexander P. Bruno, Vanderbilt University School of Medicine, Nashville, TN, United States; Rachel Harris, Monroe Carell Jr Children's Hospital at Vanderbilt, Brentwood, TN, United States; David W.. Bearl, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States

Alexander P. Bruno, BS
Medical Student
Vanderbilt University School of Medicine
Nashville, Tennessee, United States
Presenting Author(s)
Background: Previous studies have demonstrated that patients born with single ventricle heart defects have increased mortality and morbidity when there is also the presence of total anomalous pulmonary venous return (TAPVR). Prior studies have not examined how partial anomalous pulmonary venous return (PAPVR) affects outcomes in patients with single ventricle defects.
Objective: This single-center study aims to compare outcomes between single ventricle patients with TAPVR or PAPVR.
Design/Methods: We performed an IRB approved retrospective cohort study of children born between 01/2005 – 09/2023 and treated at our institution as a newborn with congenital single ventricle cardiac defect and abnormal pulmonary venous connections (as defined by imaging or surgical findings). Patients with ICD-9 or ICD-10 codes matching diagnoses of interest were identified via the Research Derivative. Data collected included demographics, diagnoses, surgical procedures, and outcomes (primary – survival, secondary – ECMO, transplant, stroke). Statistical analysis was conducted via Fisher exact test, two sample t-test, and log-rank test, as appropriate.
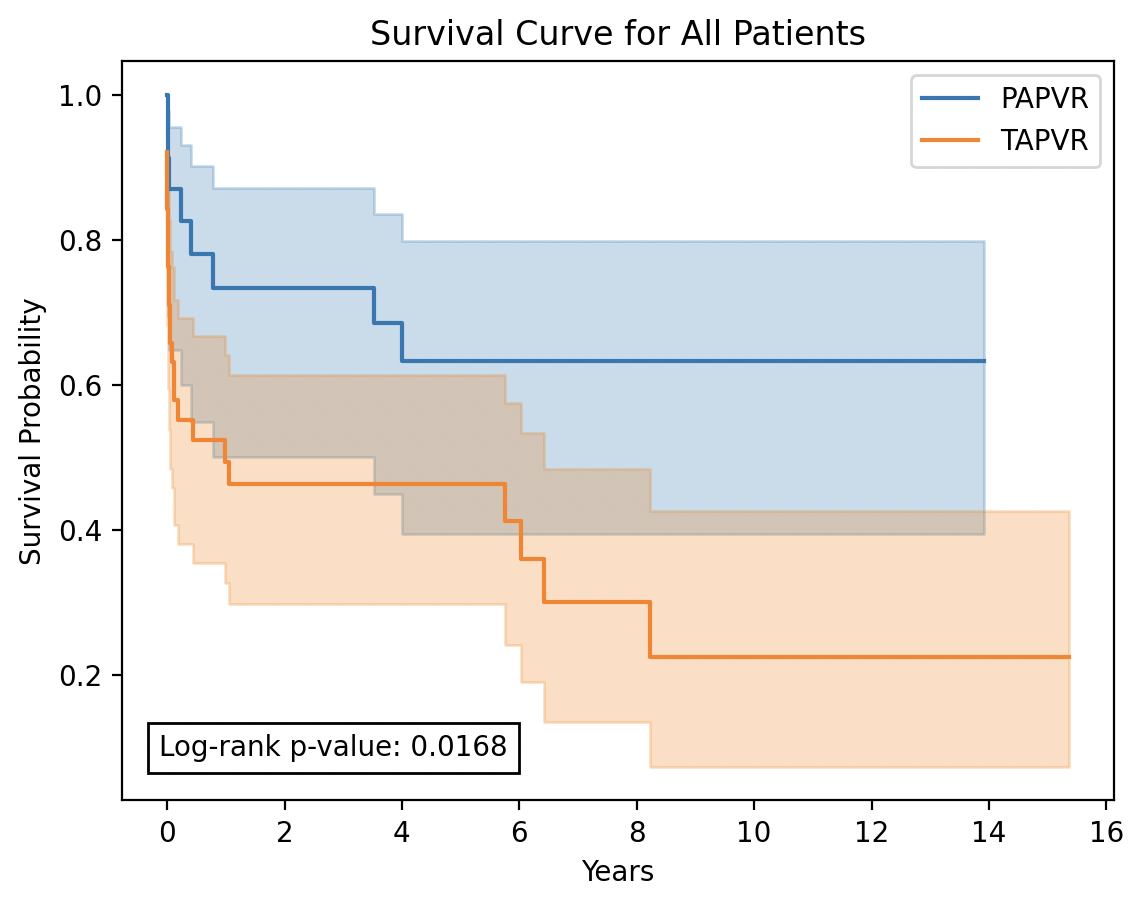
Results: Sixty-one patients were included in the analysis. Twenty-three patients had PAPVR (38%) and 38 patients had TAPVR (62%). The most common single ventricle defects included double outlet right ventricle (57%), unbalanced atrioventricular septal defect (38%), and hypoplastic left heart syndrome (36%). PAPVR patients had larger birth weights (3.39kg vs. 3.10kg, p=0.015) and were less likely to have obstructed pulmonary veins (4% vs. 45%, p=0.001). Ten PAPVR patients (43%) and 26 TAPVR patients (68%) had heterotaxy, although this difference was not statistically significant (p=0.066). Fifteen patients (25%, 3 PAPVR, 12 TAPVR, p=0.133) were deemed inoperable and received no treatment. 10-year survival was significantly better for the PAPVR cohort compared to the TAPVR cohort (63% vs 23%, p=0.017). No significant difference was found between groups for rates of ECMO, transplant, or stroke.
Conclusion(s): Single ventricle patients with PAPVR have better survival compared to those with TAPVR throughout the staged palliative process. A large multicenter study is necessary to further define operative outcomes and long-term survival in this population.
Table 1. Patient Characteristics
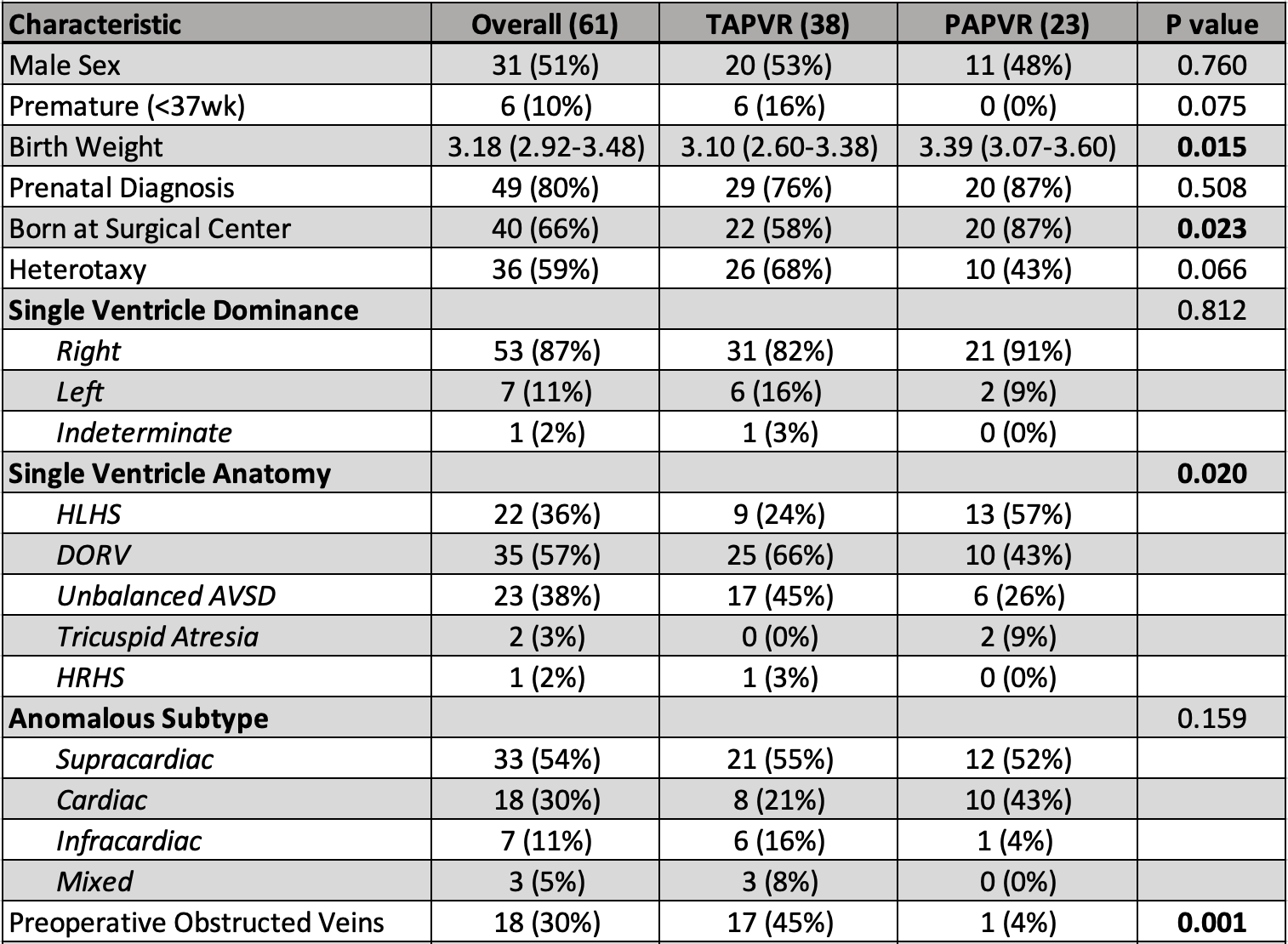 Values are median (IQR) or n (%). P-value from two-sample t-test for continuous variables or Fisher exact test for categorical variables.
Values are median (IQR) or n (%). P-value from two-sample t-test for continuous variables or Fisher exact test for categorical variables.Figure 1. Survival of Single Ventricle Patients with PAPVR or TAPVR
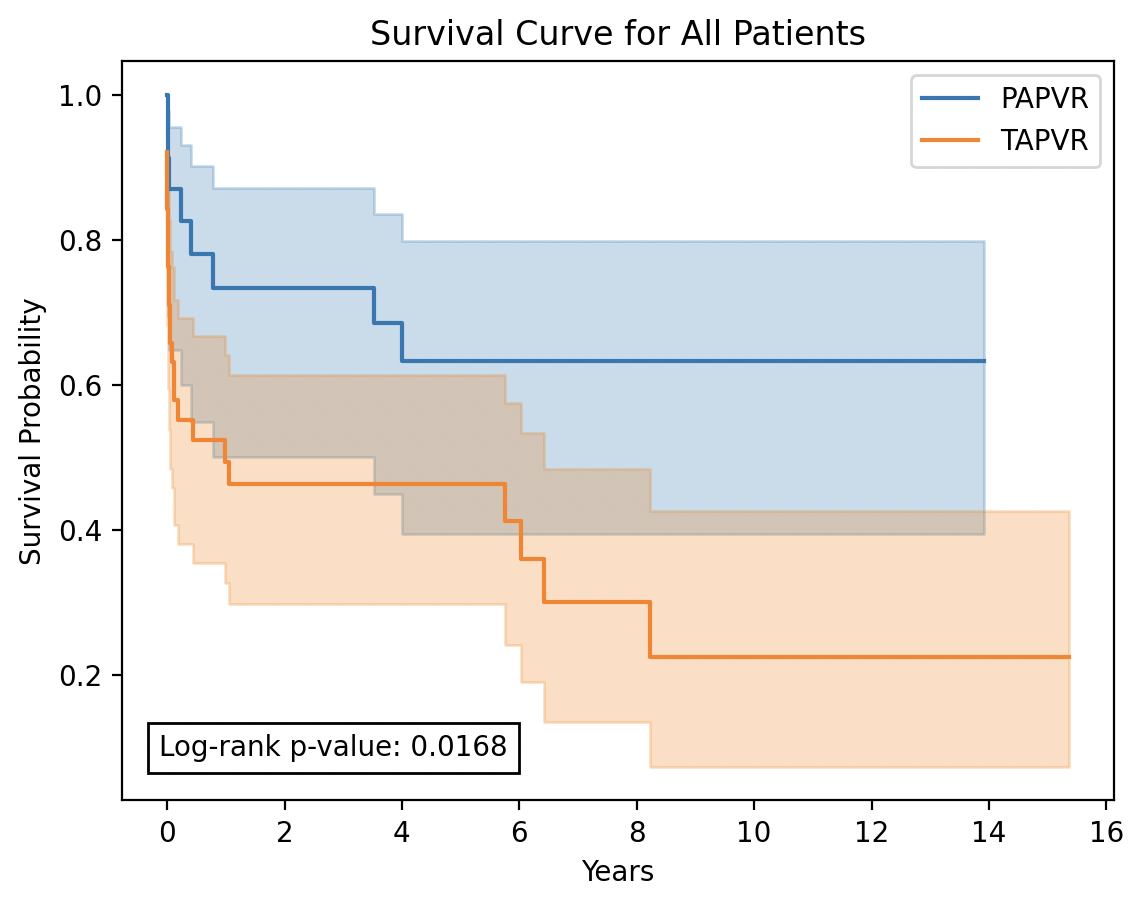
Table 1. Patient Characteristics
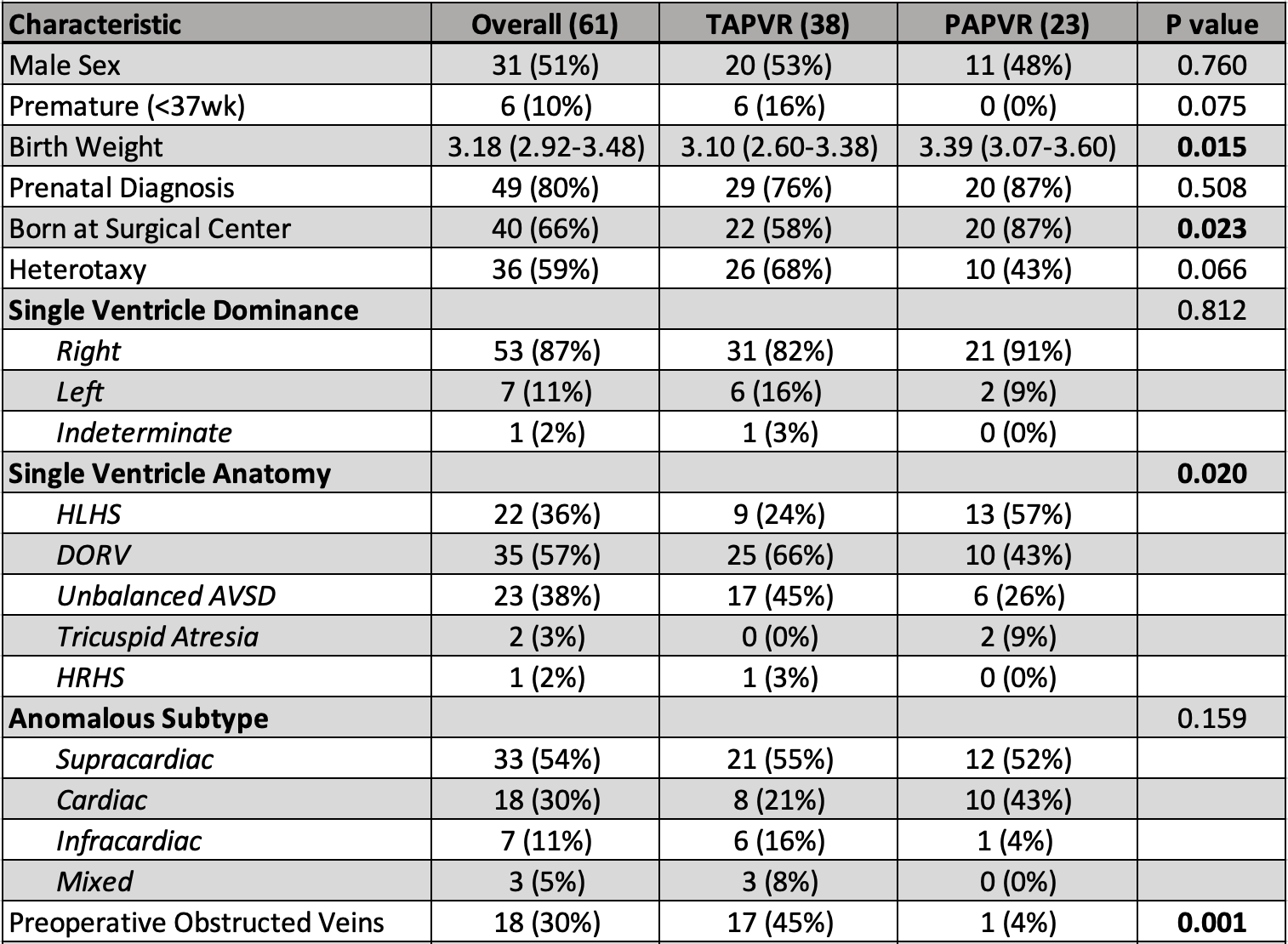 Values are median (IQR) or n (%). P-value from two-sample t-test for continuous variables or Fisher exact test for categorical variables.
Values are median (IQR) or n (%). P-value from two-sample t-test for continuous variables or Fisher exact test for categorical variables.Figure 1. Survival of Single Ventricle Patients with PAPVR or TAPVR