Neonatal Quality Improvement 3
Session: Neonatal Quality Improvement 3
086 - Improving neurologic care for neonates: implementation of a teleneurology service for extremely premature infants in the NICU
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 86.5406
Jan Martin, University of Washington School of Medicine, Seattle, WA, United States; Sarah E. Kolnik, University of Washington - Seattle Children's Hospital, Seattle, WA, United States; Niranjana Natarajan, University of Washington School of Medicine, Seattle, WA, United States
- SK
Sarah E. Kolnik, MD, MBA (she/her/hers)
Assistant Professor
University of Washington - Seattle Children's Hospital
Seattle, Washington, United States
Presenting Author(s)
Background: Neurologic complications are common in the neonatal intensive care unit (NICU) and can lead to significant neurodevelopmental sequelae. Access to neurologists is often limited to regional centers, requiring transfer of infants or consultation after discharge. Telemedicine is an effective way to examine and manage NICU patients with neurologic diagnoses. Extremely preterm infants (EPI) born at 22 0/7 – 24 6/7 weeks have a high risk of neurologic complications, and information is limited on how telemedicine can improve access to this group in regional NICUs.
Objective: By July 2025, we aim to increase the percent of EPI receiving neurology consults by 50% and decrease the time to consultation by 50% using teleneurology.
Design/Methods: This is a single center quality improvement project in a Level III/IV regional NICU affiliated with an academic medical center. A multidisciplinary team of neurologists and neonatologists formed and created a driver diagram (Figure 1). IRB-approved demographic, consult, and outcome data of EPI was retrospectively obtained from the electronic medical record. Primary outcome measure was percent of EPI admissions with neurology consult that was assessed by p-chart. The secondary outcome measure was time to neurology consultation. Baseline data was collected 01/01/22-6/30/24, when consults were available only in-person and 1-2 times a week. First Plan-Do-Study-Act (PDSA) cycle was the initiation of teleneurology services 5 days a week that began 7/1/2024. Second PDSA cycle was a guideline for when neurology consults in EPI should occur.
Results: From 2022-2024, a mean of 23 infants annually were admitted to the EPI program. Of those, neurology consulted on 18 (31%) (Figure 2), including all infants with significant intraventricular hemorrhage (IVH) (Table 1). The mean time from identification of IVH and need for neurology consultation to in-person neurology consult was 4 days (range 1-7), with 3 infants receiving only phone advice. In the four months since the implementation of our telemedicine program, Neurology has consulted on 60% of EPI with mean time to consult of 3 days (range 1-5), including all infants with significant IVH (Table 1).
Conclusion(s): The utility of neurologic consultation in the setting of complications of prematurity, such as IVH, is apparent. Given the high-risk for neurodevelopmental sequalae in all EPI, there is opportunity to improve access to timely neurology consultation through teleneurology. Further PDSA cycles to assess efficacy of teleneurology consultation in EPI is necessary, including parental satisfaction as a balancing measure.
Figure 1: Key Driver Diagram
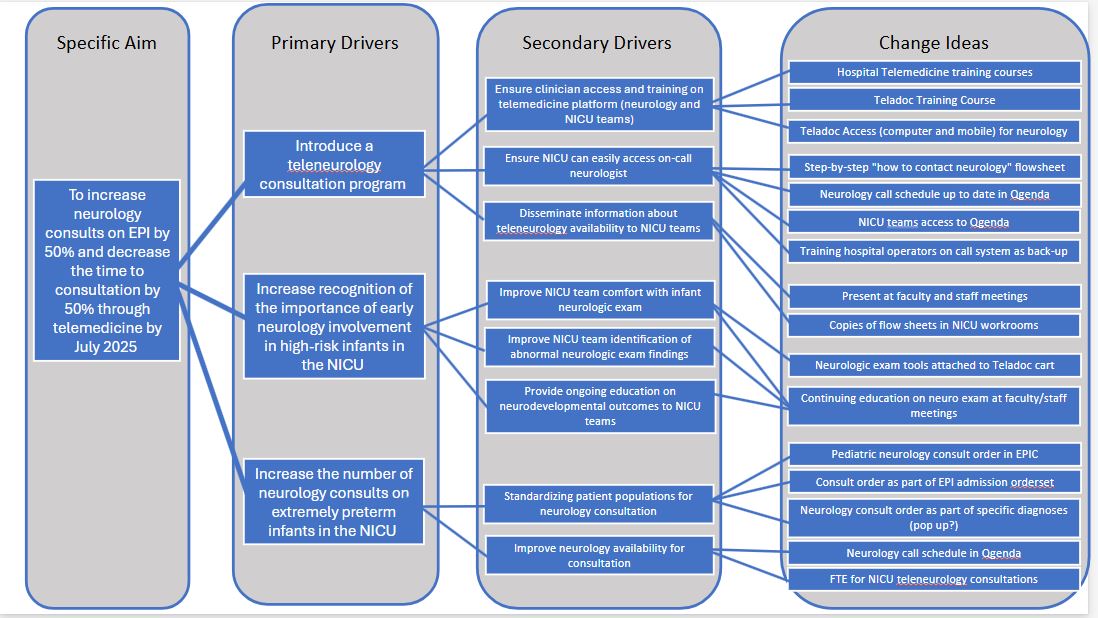
Figure 2: P-chart of EPI with neurology consultation
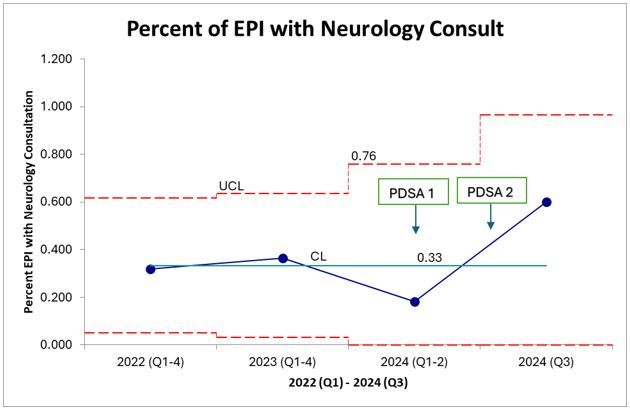 Sixty percent of EPI received neurology consult in Q3 of 2024 after implementation of teleneurology services (PDSA 1) and specification of when to get consult via guideline documentation (PDSA 2), an 80% increase from baseline of 33%.
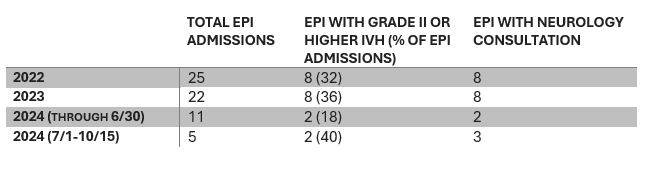
Sixty percent of EPI received neurology consult in Q3 of 2024 after implementation of teleneurology services (PDSA 1) and specification of when to get consult via guideline documentation (PDSA 2), an 80% increase from baseline of 33%. Table 1: EPI admissions and neurology consultations during the study period