Neonatal Quality Improvement 1
Session: Neonatal Quality Improvement 1
060 - Increasing Human Milk Use in the Neonatal Intensive Care Unit
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 60.5402
Jennifer B. Fundora, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Julie Murphy, Johns Hopkins Hospital, Timonium, MD, United States; Laura Wilson, Johns Hopkins Children's Center, Hanover, MD, United States; Olivia Lounsbury, Johns Hopkins Children's Center, Baltimore, MD, United States; Heidi Lochen, Johns Hopkins Children's Center, Baltimore, MD, United States; Maureen M.. Gilmore, MD, Johns Hopkins University School of Medicine, Towson, MD, United States; Michelle Gontasz, Johns Hopkins University School of Medicine, Baltimore, MD, United States
- JF
Jennifer B. Fundora, MD
Assistant Professor
Johns Hopkins University School of Medicine
Baltimore, Maryland, United States
Presenting Author(s)
Background: Human milk has immense benefits including decreased risk of acute infections, chronic illnesses, and sudden infant death syndrome (SIDS). Preterm infants fed human milk have decreased risk of necrotizing enterocolitis, chronic lung disease, and improved neurodevelopment. In a level IV NICU, baseline data 1/2022 to 12/2022 of infants discharged on human milk was 71%. It decreased in 1/2023 to 67%, below goal and decreasing, serving as an impetus for this work.
Objective: The goal of this quality improvement (QI) project is to increase human milk provision from 67% to ≥80% of neonates discharged from the NICU by 1/2026.
Design/Methods: Multiple stakeholders (lactation consultants, nurses, neonatologists, nurse practitioners, pediatric trainees, dieticians, social workers, and parents) convened. QI tools such as a fishbone diagram, key driver diagram, and parent journey mapping were utilized to identify barriers and develop interventions. The outcome measure was the proportion of infants discharged from the NICU on any human milk. Lactation consults within 72 hours of admission was a process measure. Data was followed using a statistical process control (SPC) chart.
Results: Barriers to human milk provision in the NICU included: 1) Parent support and education, 2) Accessible lactation resources and staff, and 3) Communication amongst team members regarding parental feeding preferences and education. We developed a multi-faceted approach with multiple interventions in serial PDSA cycles. Interventions include increased lactation providers, automatic consults, new breastfeeding champions program (nurses with specialized NICU lactation training), an increase in hospital grade pumps by over 50%, and increased loaner pumps for home use. The proportion of infants discharged on breastmilk increased to 72% in the last 14 months (Figure 1). We remain below goal of 80%, though we reached our goal in April 2024 for the first time in > 5 years, with ongoing interventions planned. Visits by lactation consultants within 72 hours of NICU admission increased substantially (Figure 2).
Conclusion(s): Using a QI approach, a multi-disciplinary workgroup identified several themes to increase human milk use in the NICU. Access, availability, and education of lactation resources is critical to support lactating parents and the feeding relationship with their infant. Invaluable knowledge was gained from parent journey mapping sessions, and we are developing a lactation-specific parent resource as a result. Further, we are actively evaluating parent feedback through a parent survey to inform future PDSA cycles.
Figure 1
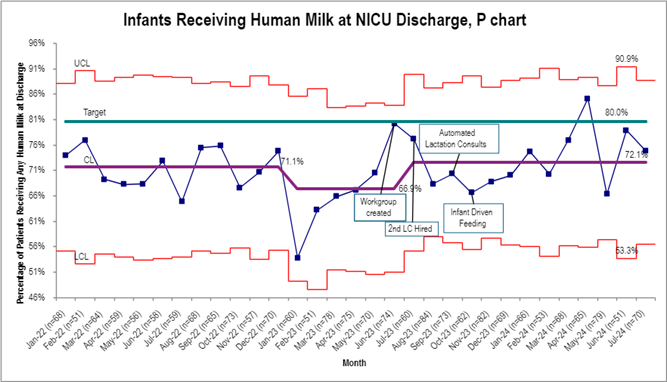 Proportion of infants discharged from the NICU receiving any human milk.
Proportion of infants discharged from the NICU receiving any human milk. Figure 2
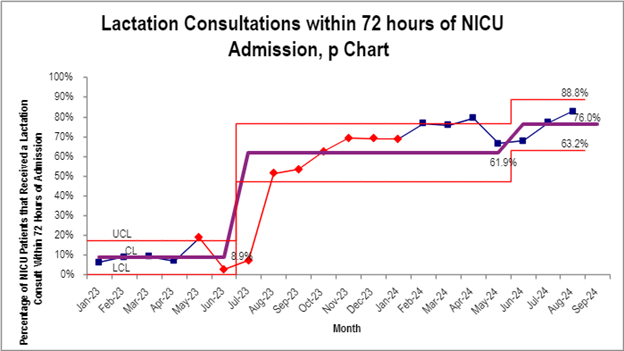 Proportion of infants with lactation visit within 72 hours of admission
Proportion of infants with lactation visit within 72 hours of admission

