Emergency Medicine 1
Session: Emergency Medicine 1
413 - Implementing Physician Breaks in a Pediatric Emergency Department
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 413.5400
Tatyana Vayngortin, Rady Children's Hospital San Diego, SAN DIEGO, CA, United States; Adnan Mesiwala, Rady Children's Hospital San Diego, San Diego, CA, United States; Fareed Saleh, University of California San Diego, SAN DIEGO, CA, United States; Scott Herskovitz, Rady Children's Hospital San Diego, San Diego, CA, United States; Clarissa M.. Angulo, Rady Children's Hospital San Diego, San diego, CA, United States; Amy Bryl, Rady Children's Hospital San Diego/University of California San Diego, San Diego, CA, United States

Tatyana Vayngortin, MD
Associate Clinical Professor
Rady Children's Hospital San Diego
SAN DIEGO, California, United States
Presenting Author(s)
Background: Many industries recognize the importance of breaks at work for optimizing performance and reducing errors. Pediatric emergency medicine (PEM) physicians work in a fast-paced environment without scheduled breaks or meals, and physiological needs may impact their cognitive performance.
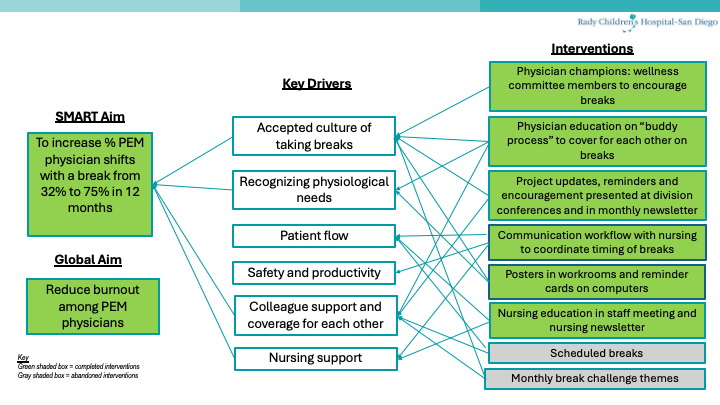
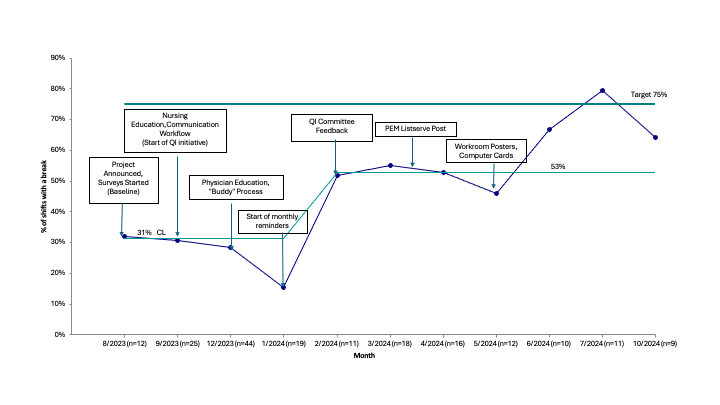
Objective: Our SMART aim was to increase the proportion of PEM physician shifts with a break from 32% to 75%, and to increase the proportion of shifts with a meal from 53% to 75% in 12 months.
Design/Methods: Plan-Do-Study-Act (PDSA) cycles began in August 2023. We collected baseline data by surveying physicians about the percentage of shifts in the past week in which they took a break , as well as enablers and barriers to taking breaks. We defined a break as 15 minutes away from clinical care during a shift. A key driver diagram displayed our drivers and interventions (Figure 1). We collaborated with nursing leadership to create a communication workflow for timing of physician breaks to avoid patient overflow in zones, and educated nurses on this process. We implemented a “buddy process” in which physicians working in the same zone of the emergency department (ED) would cover for each other during breaks. We shared monthly reminders at division conference and via an electronic newsletter, and posted reminder posters around the ED. Electronic surveys were sent to the physicians monthly to track measures. The primary measure was the percentage of shifts in the past week with a break. Secondary outcome measures included the percentage of shifts in the past week with a meal, and well-being scores measured on an annual division survey. Balancing measures included productivity measures, such as patients per hour and relative value units per hour. Pre and post intervention measures were analyzed using statistical process control.
Results: Within 6 months of the start of the quality improvement (QI) initiative, the percentage of shifts with a break increased from 32% to 53% (Figure 2). Within 11 months, the goal of 75% was attained. Within 5 months, the percentage of shifts with a meal increased from 53% to 71% (Figure 3), and the goal of 75% was reached on several months. Job satisfaction scores on a well-being survey increased by 23%, and physician productivity did not decrease.
Conclusion(s): Using QI methods to identify barriers to PEM physicians taking breaks on shift, we increased the proportion of shifts with a break from 32 to 53%, and shifts with a meal from 53 to 71%. We found that building a culture where breaks for physicians are accepted requires time, encouragement, and support from physician and nursing colleagues.
Key Driver Diagram
Run p Chart of Breaks on Shift
Run p Chart of Meals on Shift
.png)


