Neonatal Quality Improvement 2
Session: Neonatal Quality Improvement 2
074 - Intervention effectiveness in reducing the time to discharge for patients with Neonatal Opioid Withdrawal Syndrome at a large county hospital
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 74.5376
Tenzin Palkyi, University of Texas Southwestern Medical School, Dallas, TX, United States; Colleen J.. Bonner, Parkland Health, Dallas, TX, United States; Maria G. Ruvalcaba Parra, Parkland Health, Dallas, TX, United States; Jamie L. Walker, Parkland Health and Hospital Systems, Dallas, TX, United States; Kristen Dawson, University of Texas Southwestern Medical School, Richardson, TX, United States; Tara Best, Parkland, Dallas, TX, United States; Kathryn G. Mazioniene, University of Texas Southwestern Medical School, Fort Worth, TX, United States; Venkatakrishna Kakkilaya, UT Southwestern Medical Center, Dallas, TX, United States; Lorraine Bautista, University of Texas Southwestern Medical School, Dallas, TX, United States
- TP
Tenzin Palkyi, BS BSA (she/her/hers)
MD Candidate
University of Texas Southwestern Medical School
Dallas, Texas, United States
Presenting Author(s)
Background: Recent increases in chronic opioid use, including among pregnant patients, have led to a rise in neonatal opioid withdrawal syndrome (NOWS). The lack of standardized care for NOWS patients has caused variability in clinical outcomes, treatment duration, and discharge times. At a local large county hospital, discharge times average 4 days—longer than the recommended 48-72 hours.
Objective: To assess the effectiveness of improved discharge-date communication and multidisciplinary round attendance in decreasing median time to discharge of infants with NOWS from 4 to 2 days.
Design/Methods: The outcome measure was the median time to discharge following NOWS treatment. The process measure was the percentage of neonatal ICU staff who utilized the intervention, and readmission rate for NOWS symptoms was the balancing measure. The DMAIC (Define-Measure-Analyze-Improve-Control) methodology was employed. Literature review and NICU staff interviews comprised the Define stage, while retrospective chart review from discharge data (January 2020- August 2022) served as the Measure step. The Analyze phase consisted of QI tool development such as swimlane and driver diagrams. The area of focus for this intervention based on data analysis was discharge date communication. A PDSA (Plan-Do-Study-Act) cycle from September 2022-January 2024 then targeted weekly multidisciplinary NICU discharge rounds attendance, updated documentation in daily notes by providers and social workers regarding discharge disposition, and expected date of discharge.
Results: Prior to September 2022, 122 NOWS patients had a mean time to discharge of 3.01 days and a median of 4 days. After September 2022, there were 58 total patients with NOWS; the mean time to discharge decreased to 2.64 days while the median was 2 days, demonstrating a 12% improvement in mean time to discharge and a 50% improvement in median time for the outcome measure. For the process measure, there was a 245% cumulative increase in the attendance rate at multidisciplinary rounds by staff members involved in the QI initiative. Lastly, the readmission rate remained at 0% over the course of the PDSA cycle duration.
Conclusion(s): This initiative highlights the complexity of NICU discharge, emphasizing the need for team foresight to minimize unnecessary length of stay after treatment completion. Adhering to 48-hour discharge guidelines can be facilitated by strengthening multidisciplinary rounds attendance, prioritizing patients with approaching discharge dates, and enhancing communication with supporting services and Child Protective Services when applicable.
Figure 1: Key Driver Diagram
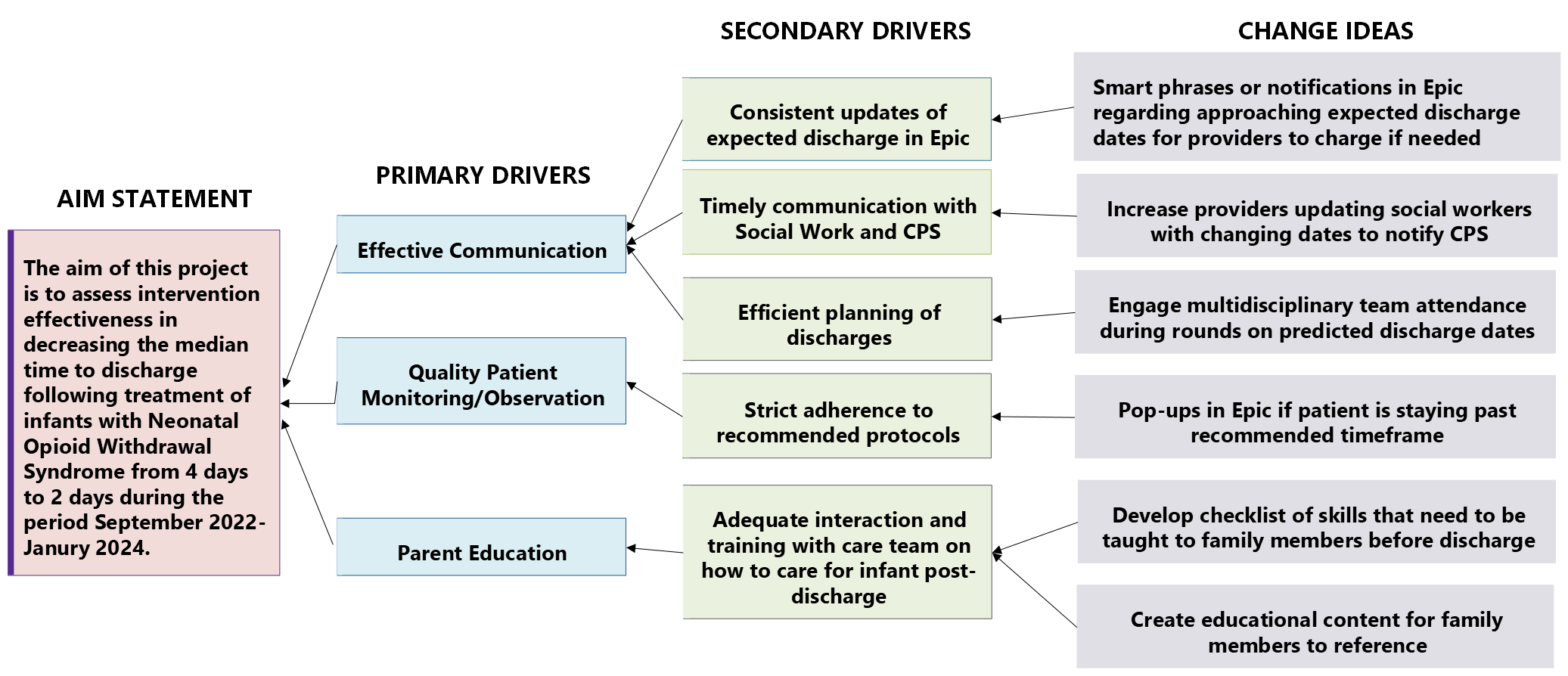 This driver diagram displays the relationship between the aim of the original project, primary and secondary drivers, and possible interventions to test.
This driver diagram displays the relationship between the aim of the original project, primary and secondary drivers, and possible interventions to test.Figure 2: Swimlane Diagram
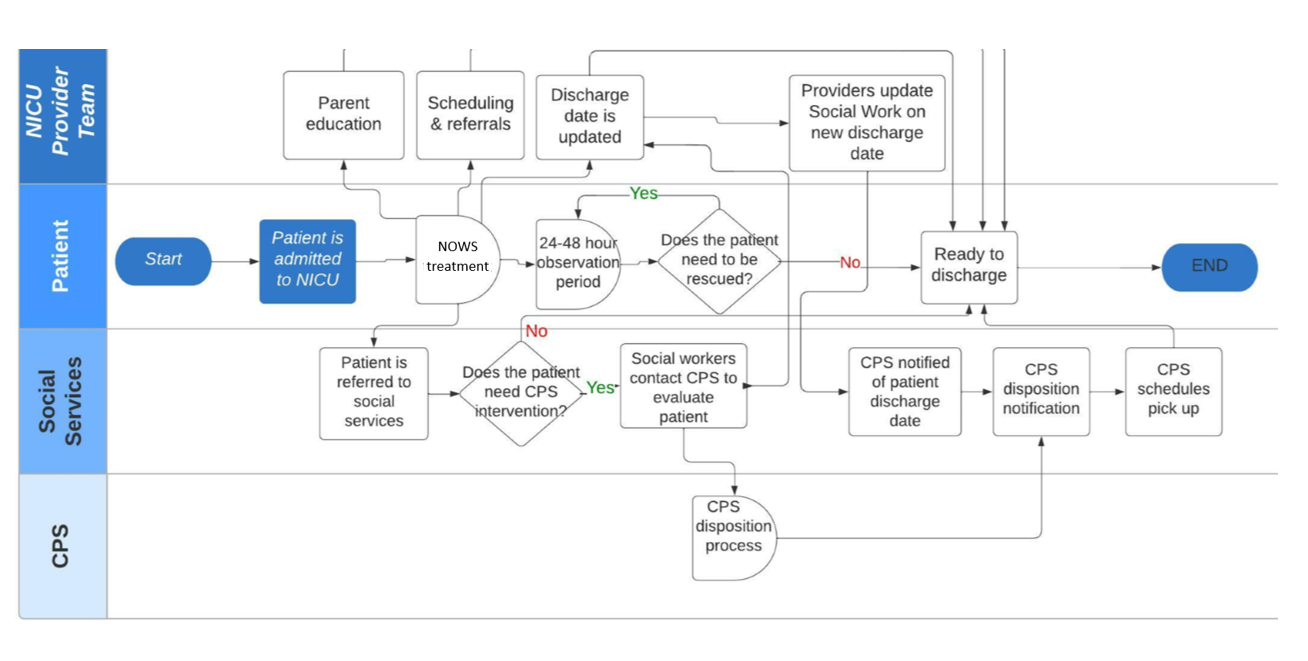 The swimlane diagram was instrumental in mapping out the current state of the discharge process after conducting interviews with NICU staff, and it indicates bottlenecks that were identified.
The swimlane diagram was instrumental in mapping out the current state of the discharge process after conducting interviews with NICU staff, and it indicates bottlenecks that were identified.Table 1: Primary Results
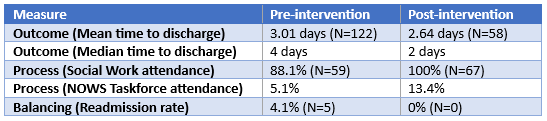 This table summarizes the main results for the primary outcome, process, and balancing measures for patients with NOWS regarding various elements of their discharge process.
This table summarizes the main results for the primary outcome, process, and balancing measures for patients with NOWS regarding various elements of their discharge process.

