Critical Care 2
Session: Critical Care 2
126 - Pediatric Hospitalization and the Parent-Child Relationship
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 126.5708
Dianna L. Mejia, NewYork-Presbyterian Komansky Children’s Hospital, New York, NY, United States; Chani Traube, Weill Cornell Medicine, New York, NY, United States; Caroline Andy, Weill Cornell Medicine, New York, NY, United States; Linda M. Gerber, Weill Cornell Medicine, New York, NY, United States; Morgan Smith, Weill Cornell Medicine, New York, NY, United States; Samantha Bruno, Weill Cornell Medicine, New York, NY, United States; Keshia Small, Weill Cornell Medicine, New York, NY, United States; Alexandra Berardi-Bloomfield, Children's Hospital Colorado, Denver, CO, United States; Lauren Habermann, Icahn School of Medicine at Mount Sinai, Long Island City, NY, United States

Dianna L. Mejia, MD (she/her/hers)
PGY-3
NewYork-Presbyterian Komansky Children’s Hospital
New York, New York, United States
Presenting Author(s)
Background: A child’s hospitalization is disruptive for the entire family and effects can persist after discharge home. There is limited research as to how a child’s hospitalization may impact parenting and the parent-child relationship.
Objective: Primary objective is to measure parenting self-efficacy (PSE) in parents of recently hospitalized children. PSE refers to a parent's confidence in ability to effectively manage parenting tasks (e.g. attachment, communication, discipline, involvement, and overall parent-child relationship). A secondary objective is to identify family factors associated with PSE after discharge.
Design/Methods: In this prospective cohort study, participants include parents of patients 2-18 years old who were admitted to the hospital for >2 nights. Two weeks after discharge, parents received a computerized link to complete the BASC-3 Parenting Relationship Questionnaire (PRQ). Parental scores on each domain were compared to the national average. Kruskal-Wallis rank sum tests assessed domain-specific parenting scores by family characteristics (e.g. religiosity, siblings, prior hospitalization, parent history of mental illness).
Results: 1268 parents were contacted; 214 (17%) responded; 182 (85%) completed the PRQ. Compared to the national average, the overall cohort reports less confidence in their ability to discipline their child (PSE score 20 vs. 50, p< 0.001) and more involvement in their child’s lives (63 vs. 50, p< 0.001) (Fig 1). Families who describe themselves as religious score higher on communication (65 vs. 32, p=0.018), and lower on discipline (16 vs. 7, p=0.007). Parents with only one child have higher overall attachment (65 vs. 51, p=0.026) and involvement (89 vs. 62, p=0.004), and less frustration (37 vs. 51, p=0.04), than families with siblings. Parents with a history of mental health issues report lower scores on attachment (40 vs. 58, p=0.009) and overall parenting confidence (31 vs. 54, p=0.033). There is no difference in PSE domain scores from the national average among families where the child had a previous admission. Exploratory factor analysis (EFA) identifies the underlying structure in the parenting domains, with 72% of variance explained by 2 factors (Fig 2).
Conclusion(s): Parents report lower efficacy in parenting after a child’s first hospitalization, with marked effects on discipline practices when compared to national norms. Parents with a prior mental health diagnosis, more than one child, and without religious affiliation may benefit most from interventions designed to increase PSE after hospital discharge.
Table 1. Family Characteristics
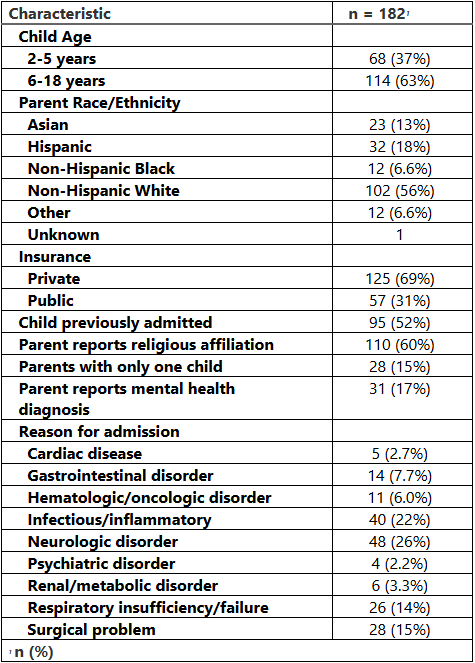
Figure 1. Average Parenting Relationship Questionnaire Scores by Domain: Sample vs. National Data
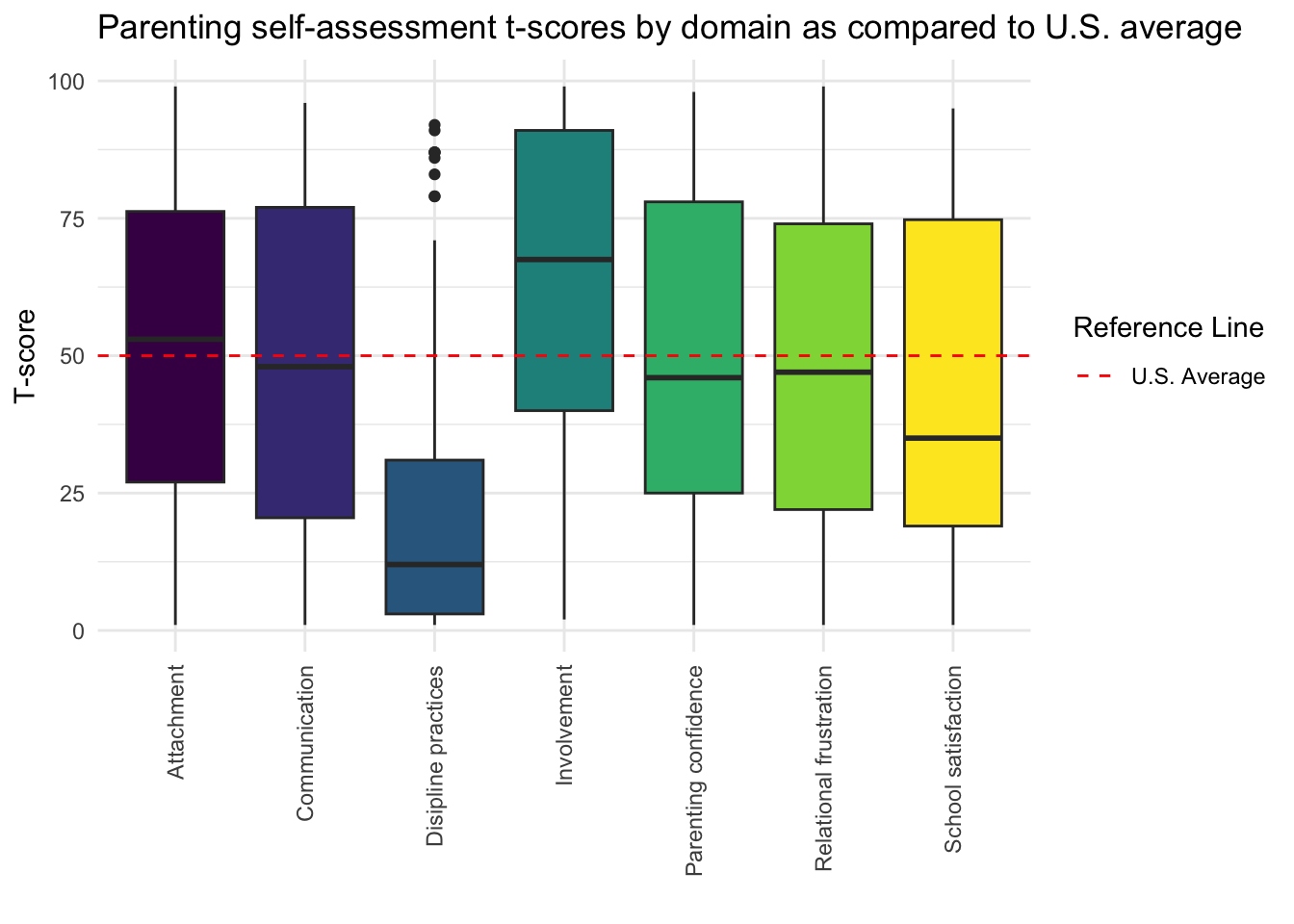
Figure 2. Exploratory Factor Analysis and Underlying Structure in Parenting Domains
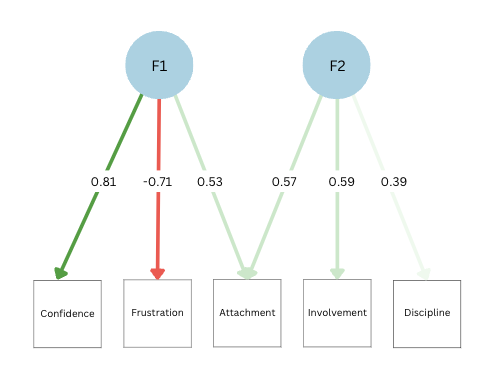 Factor 1 is characterized by high loadings from measures of attachment (0.53), parenting confidence (0.81) and low frustration (-0.71); Factor 2 exhibits strong loadings from attachment (0.57) and involvement (0.59).
Factor 1 is characterized by high loadings from measures of attachment (0.53), parenting confidence (0.81) and low frustration (-0.71); Factor 2 exhibits strong loadings from attachment (0.57) and involvement (0.59). 
