Neonatal Hemodynamics and Cardiovascular Medicine 1
Session: Neonatal Hemodynamics and Cardiovascular Medicine 1
200 - Outpatient Cardiology Follow-up Among Extremely Preterm Infants Discharged with a Hemodynamically-Significant Patent Ductus Arteriosus
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 200.5654
Valerie Kirtley, Nationwide Children's Hospital, Columbus, OH, United States; Brian Rivera, The Abigail Wexner Research Institute at Nationwide Children's Hospital, Columbus, OH, United States; Lauren Capaci, Nationwide Children's Hospital, Columbus, OH, United States; Lillian Holloway, The Abigail Wexner Research Institute at Nationwide Children's Hospital, Columbus, OH, United States; Carl Backes, Nationwide Children's Hospital, Col, OH, United States
- VK
Valerie Kirtley, MD (she/her/hers)
Resident
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background: There are no guidelines regarding best practice for outpatient cardiology follow-up among extremely preterm infants discharged with a patent ductus arteriosus (PDA).
Objective: In the absence of national guidelines, we sought to characterize outpatient cardiology follow-up practice patterns among extremely preterm infants (EPIs; < 28 weeks of gestation) with a hemodynamically significant patent ductus arteriosus (HSPDA) at time of initial hospital discharge at a large, pediatric tertiary care center.
Design/Methods: We conducted a multicenter, retrospective, observational study of EPIs during 2013 and 2023 and discharged with a HSPDA (defined as minimum ductal size >2.0 mm/kg). We identified the consistency of outpatient cardiology follow-up and need for post-discharge intervention.
Results: Two hundred and seventy-nine EPIs were discharged with a persistent PDA (Figure). Among EPIs with persistent PDA at NICU discharge, median gestational age was 25.7 weeks, median birth weight was 805 g, and median duration of hospitalization was 111 days; 157 (56.3%) infants were discharged on oxygen. Ductal size at discharge in most infants was trivial to small (251, 90.0%); 28 (10%) infants had a HSPDA at last known ECHO prior to NICU discharge. The median time (range) between last-known inpatient ECHO and discharge was 64 (2 – 145) days. Among EPIs with HSPDA, 11/28 (39.2%) were scheduled for an outpatient cardiology follow-up, of which all (11/11; 100%) were seen. Of note, 17/28 (60.8%) failed to be scheduled with an outpatient cardiology provider at time of initial discharge. Importantly, among 11 EPIs with HSPDA at initial discharge, 4 (36.3%) required percutaneous closure at a median (range) of 20 (8 -33) postnatal months.
Conclusion(s): EPIs with HSPDA at time of initial NICU discharge may require outpatient ductal closure. Therefore, efforts to provide systematic and consistent outpatient cardiology follow-up for these higher risk infants is greatly needed.
Figure
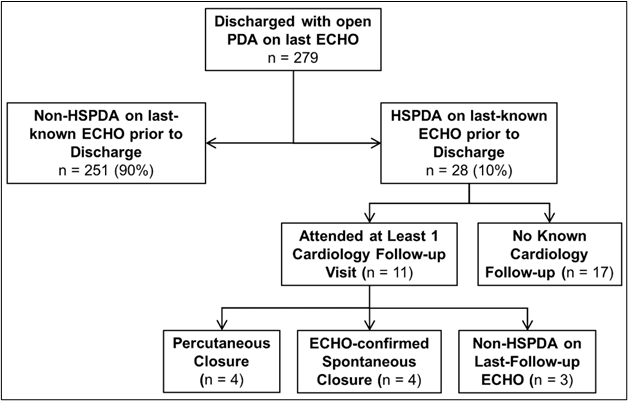 Flowchart showing follow-up incidence and outcomes among 28 extremely preterm infants with a hemodynamically significant patent ductus arteriosus on last-known echocardiogram prior to discharge.
Flowchart showing follow-up incidence and outcomes among 28 extremely preterm infants with a hemodynamically significant patent ductus arteriosus on last-known echocardiogram prior to discharge.Figure
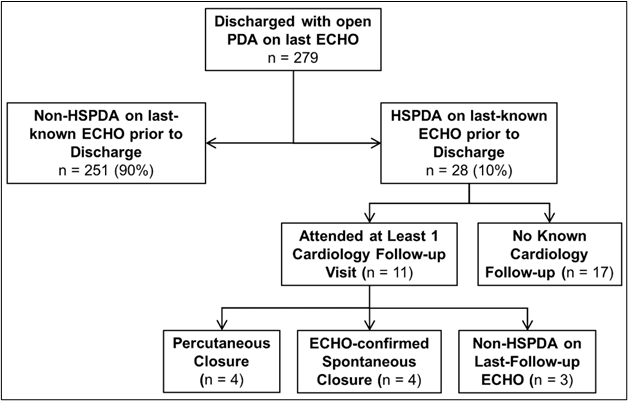 Flowchart showing follow-up incidence and outcomes among 28 extremely preterm infants with a hemodynamically significant patent ductus arteriosus on last-known echocardiogram prior to discharge.
Flowchart showing follow-up incidence and outcomes among 28 extremely preterm infants with a hemodynamically significant patent ductus arteriosus on last-known echocardiogram prior to discharge.
