Emergency Medicine 1
Session: Emergency Medicine 1
414 - Partnerships with Pediatric Academic Medical Centers: A Qualitative Needs Assessment for Pediatric Care in Northern California Community Emergency Departments
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 414.5618
Rajesh K. Daftary, University of California, San Francisco, School of Medicine, Oakland, CA, United States; Ashley Foster, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Anneka Hooft, University of California, San Francisco, School of Medicine, San Franciscio, CA, United States; Sara Malakzay, University of California, San Francisco, School of Medicine, West Sacramento, CA, United States; Peter Baker, University of California, San Francisco, School of Medicine, Ross, CA, United States; Ryman R. Crone, UCSF Benioff Children's Hospital Oakland, San Francisco, CA, United States; Le N. Lu, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Inder K. Narula, University of California, San Francisco, Greenbrae, CA, United States; Sonny Tat, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Shruti Kant, University of California, San Francisco, School of Medicine, San Francisco, CA, United States

Rajesh K. Daftary, MD, MPH (he/him/his)
Associate Professor
University of California, San Francisco, School of Medicine
Oakland, California, United States
Presenting Author(s)
Background: The majority of children in the United States seek emergency care within community emergency departments (CEDs). Community emergency departments may partner with pediatric academic medical centers (PAMC) within their region for pediatric services such as specialty consultation, follow-up, as well as patient transfers. These collaborations may be conduits for additional support of CEDs in aspects of real-time patient care support, aftercare coordination, and enhanced pediatric readiness.
Objective: We sought to explore CED experiences with care of children and their perspectives on how a PAMC can support the provision of that care.
Design/Methods: We used qualitative techniques associated with a phenomenological approach to explore lived experiences in CEDs. Purposeful sampling identified CEDs with rural and nonrural designations and those located in adjacent and nonadjacent counties to the PAMC. In semi-structured interviews with nurse and physician leadership from CEDs we asked about their experiences in caring for children and desired PAMC support. Using reflexive thematic analysis we analyzed the data and identified themes.
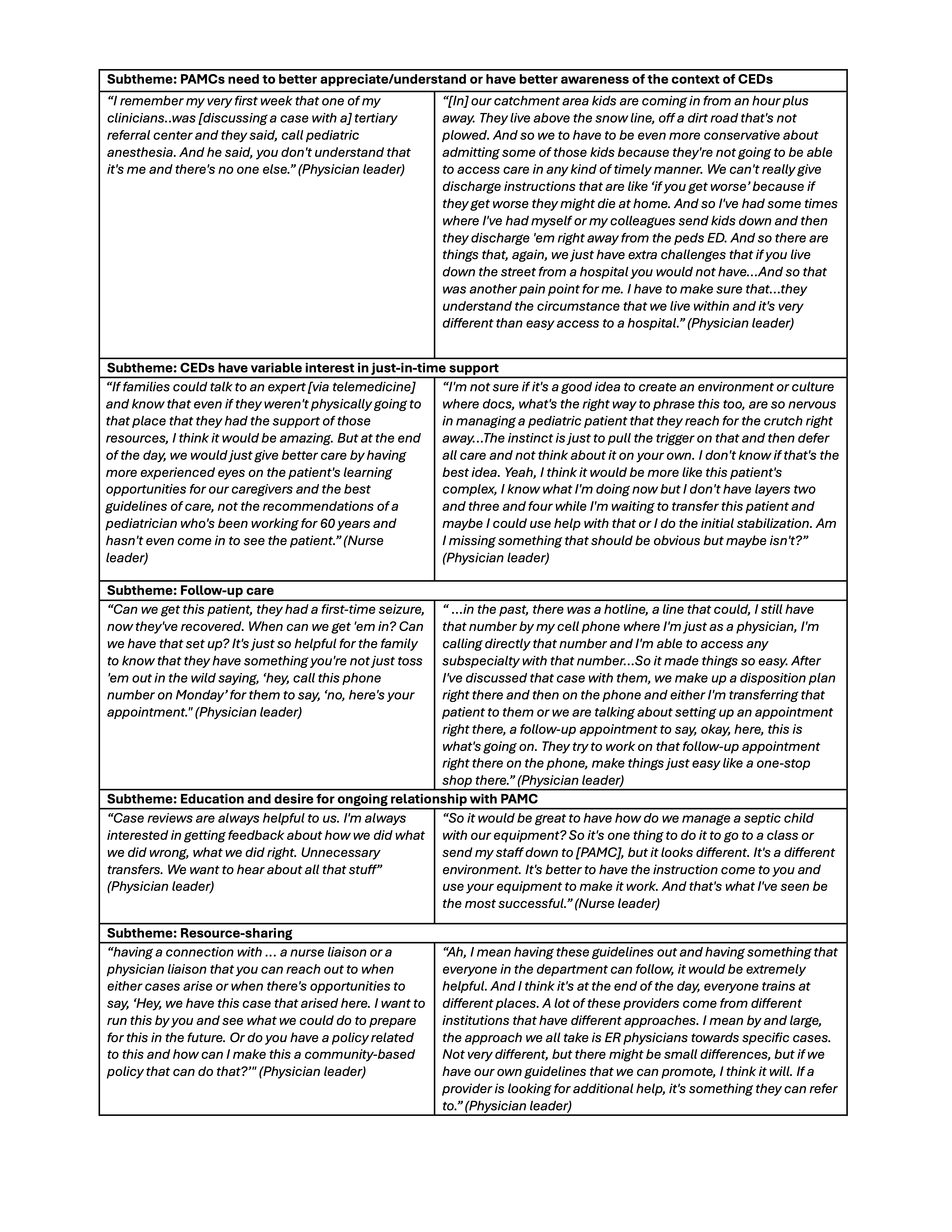
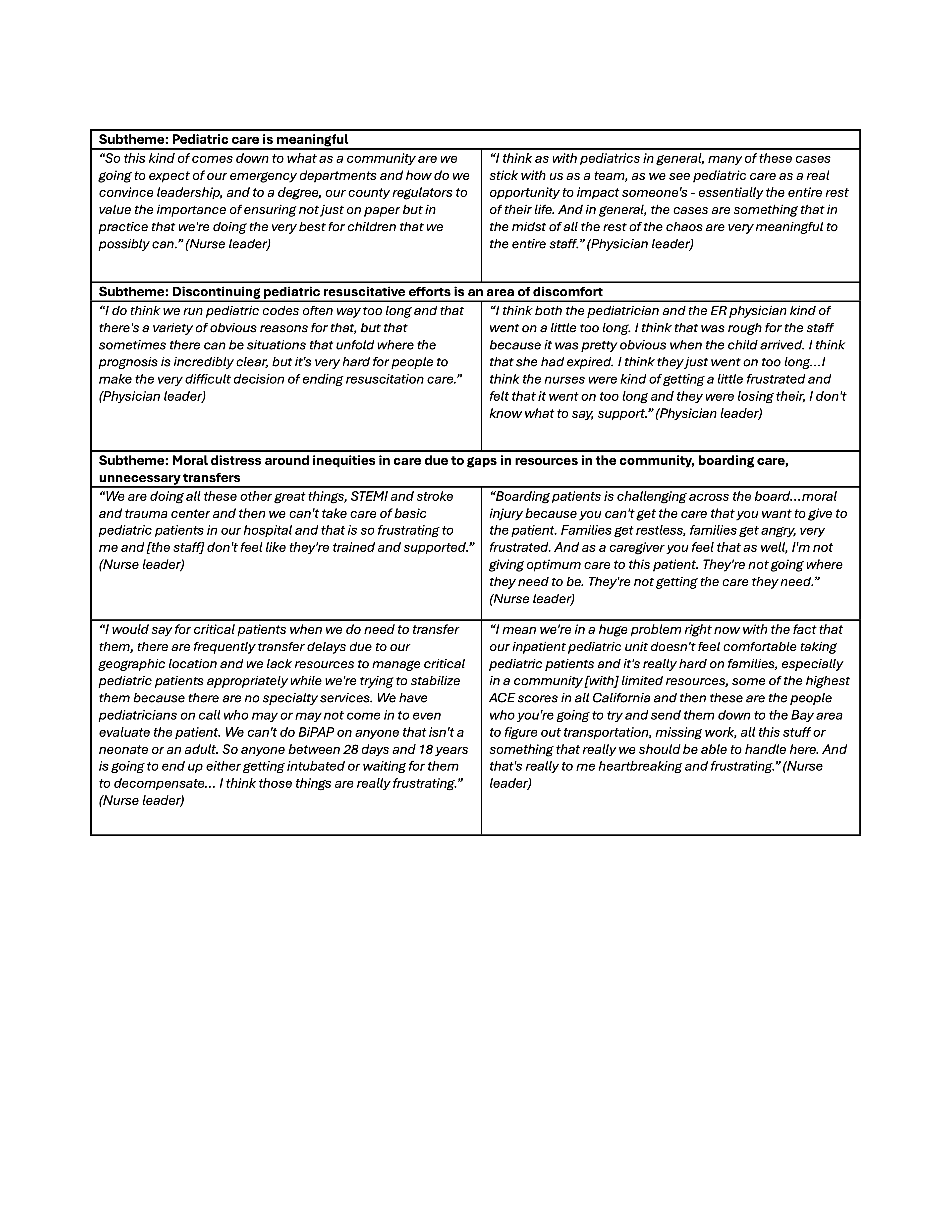
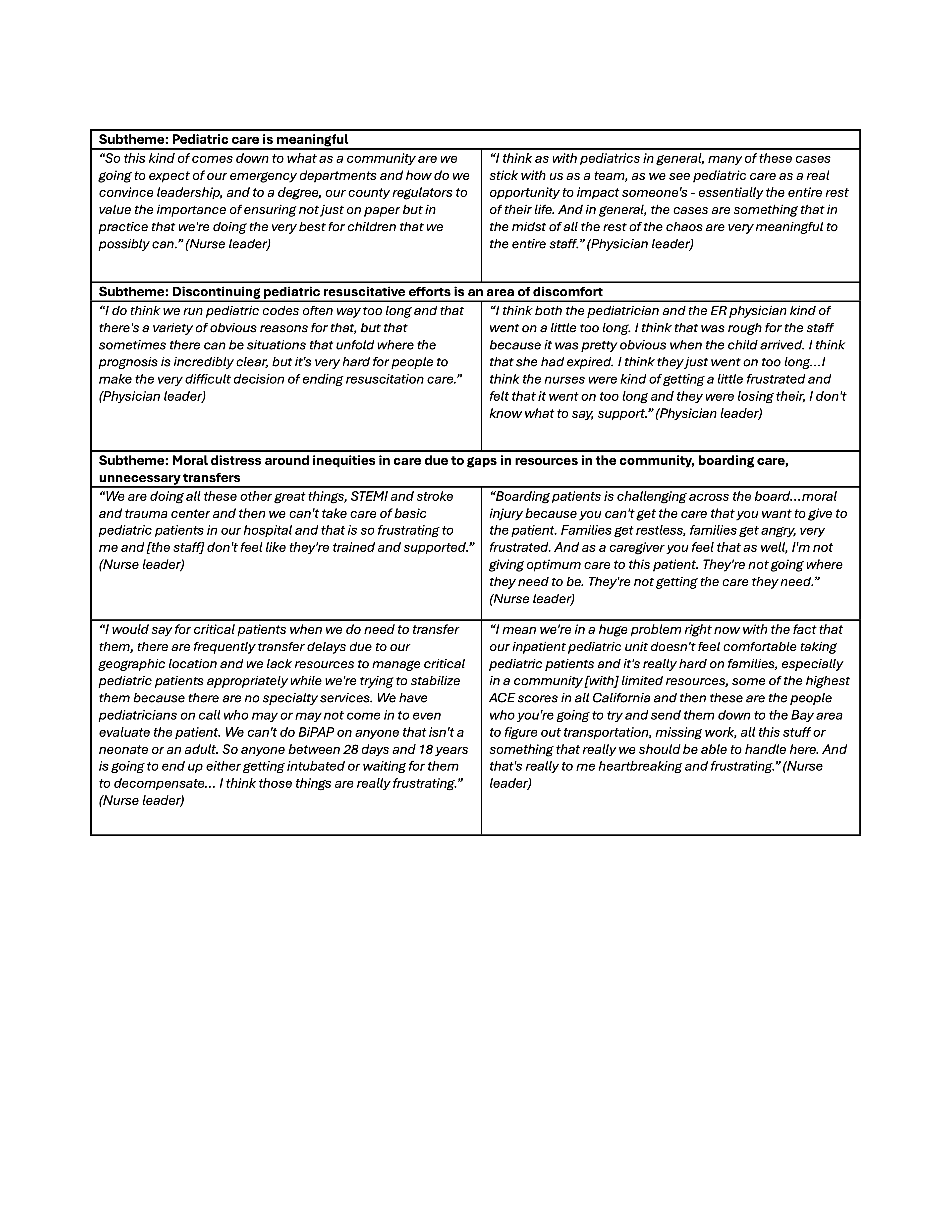
Results: We interviewed 13 nurse and 10 physician leaders representing eight CEDs (three rural, five in nonadjacent counties). In preliminary data analysis, we identified three major themes: (1) existing pediatric infrastructure impacts care (Table 1), (2) caring for pediatric patients can have an emotional impact (Table 2), and (3) opportunities for increased PAMC support for CEDs is desired/valued (Table 3). We identified subthemes for desired support which include education, just-in-time decision-making, resources to support standardization of care, and coordination of aftercare.
Conclusion(s): Our findings affirmed that CEDs value high-quality pediatric care delivery but often encounter barriers. CEDs frequently reported a loss of in-house pediatric-specific support as a barrier to care and desired partnerships with PAMCs to enhance care delivery. The type of desired resources varied across CEDs, but they frequently identified coordination of subspecialty care, facilitation of transfer, and educational support as opportunities that PAMCs can uniquely offer. These findings can be used to inform how a PAMC allocates resources to such partnerships and help close care gaps identified by CEDs.
Table 1. Existing Pediatric Infrastructure Impacts Care
.png)
Table 2. Caring for Pediatric Patients Can Have an Emotional Impact
 ACE- Adverse childhood experiences, BiPAP- Bilevel positive airway pressure, ER- emergency room
ACE- Adverse childhood experiences, BiPAP- Bilevel positive airway pressure, ER- emergency roomTable 3. Opportunities for Increased Pediatric Academic Medical Center (PAMC) Support is Desired/Valued
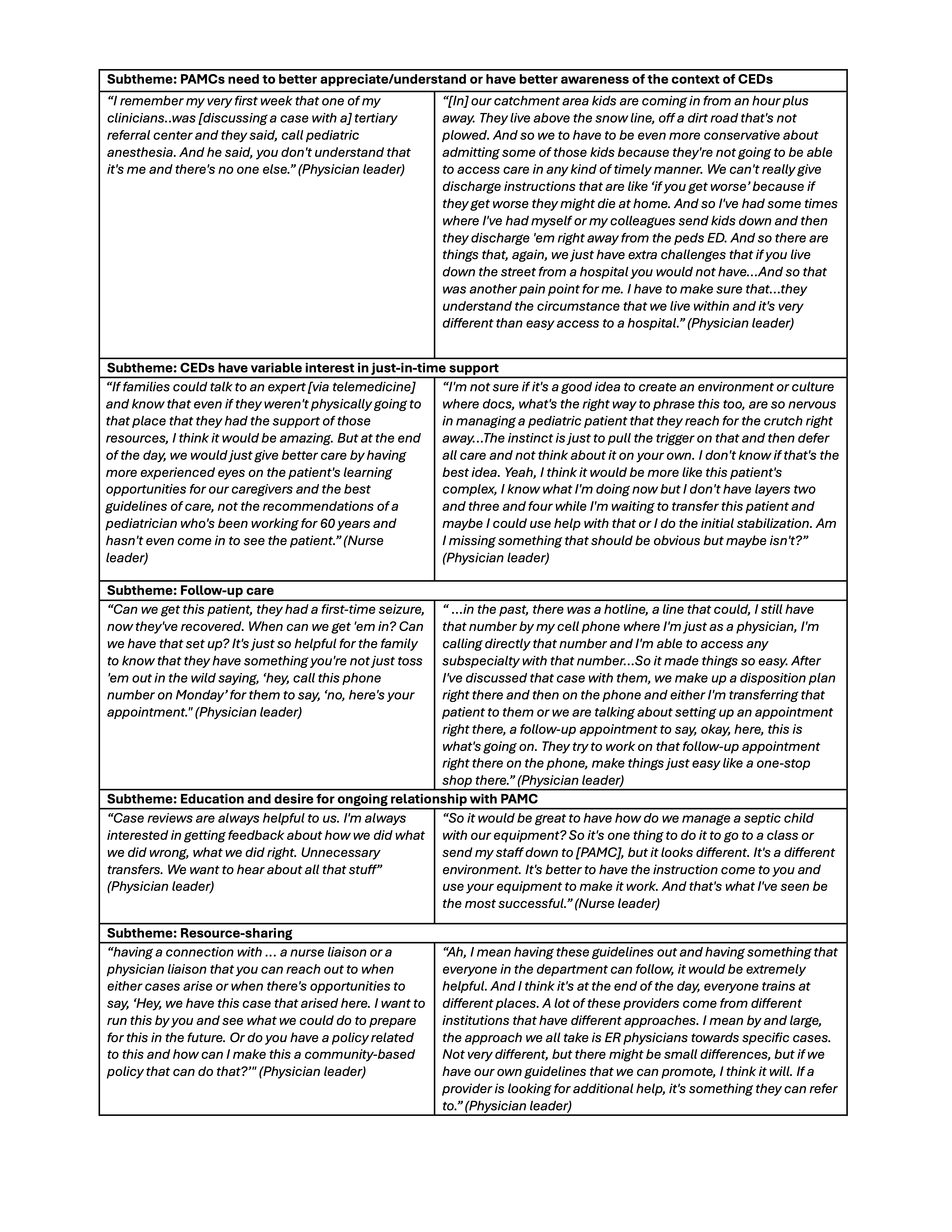
Table 1. Existing Pediatric Infrastructure Impacts Care
.png)
Table 2. Caring for Pediatric Patients Can Have an Emotional Impact
 ACE- Adverse childhood experiences, BiPAP- Bilevel positive airway pressure, ER- emergency room
ACE- Adverse childhood experiences, BiPAP- Bilevel positive airway pressure, ER- emergency roomTable 3. Opportunities for Increased Pediatric Academic Medical Center (PAMC) Support is Desired/Valued