Quality Improvement/Patient Safety 3
Session: Quality Improvement/Patient Safety 3
037 - Operationalizing automated e-trigger rate to monitor adverse events
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 37.5900
Dionne A. Graham, Boston Children's Hospital, Boston, MA, United States; Phillip D.. Hahn, Boston Children's Hospital, Boston, MA, United States; Anya Mascarenhas, Boston Children's Hospital, Boston, MA, United States; Sara Toomey, Boston Children's Hospital, Cambridge, MA, United States
- ST
Sara Toomey, MD, MPhil, MPH, MSc (she/her/hers)
Chief Safety and Quality Officer, SVP
Boston Children's Hospital
Cambridge, Massachusetts, United States
Presenting Author(s)
Background: The Global Assessment of Pediatric Patient Safety (GAPPS) trigger tool is a standardized methodology used to identify adverse events (AE) in pediatric inpatient settings by systematically reviewing patient records for specific “triggers” that indicate patient harm. While GAPPS has demonstrated ability to detect AEs not otherwise captured by voluntary reporting, the chart review process and adjudication of suspected AEs is resource intensive. Fully electronic trigger tools offer an automated, near real-time approach to safety surveillance with demonstrated ability to develop objective standardized ongoing adverse event rates and identify opportunities for timely risk mitigation. The utility of the GAPPS electronic triggers (e-triggers) as safety indicators for early detection of systems issues is unknown.
Objective: To evaluate the performance of an e-trigger rate as an automated high-level safety indicator in hospitalized pediatric patients and to identify systemic challenges to operationalizing e-triggers.
Design/Methods: Twenty of the twenty-nine GAPPS triggers are based on discrete fields in the electronic health record (EHR), making them suitable for automation. We developed SQL code to query our data warehouse identify inpatients who met criteria for each trigger on a given calendar day. We calculated the e-trigger rate, defined as the number of triggers/1,000 patient days, for all patient days in 2023, for each individual trigger and collectively across all triggers. The data were visualized over time in a web-based dashboard. We validated a subset of the triggers where gold standard lists of AEs exist.
Results: We encountered challenges with establishing the daily e-triggers, including: converting original triggers from ICD-10 diagnosis codes assigned at discharge to daily physician billing codes, triggers activating on multiple days for a single AE, inconsistent EHR documentation, and lack of trigger specificity for the occurrence of an AE. We created a dashboard to visualize e-trigger rate, enabling real time monitoring as the triggers are refined. The sensitivity and specificity of the e-triggers in identifying corresponding AE varied widely across different triggers.
Conclusion(s): This study highlighted the challenges with converting components of the GAPPS trigger tool to automated, daily AE detection. Future work will focus on refining the triggers to incorporate additional documentation in the EHR, improving accuracy and reliability including enhancing AE detection using AI.
Table 1: GAPPS e-triggers and barriers to daily operationalization.
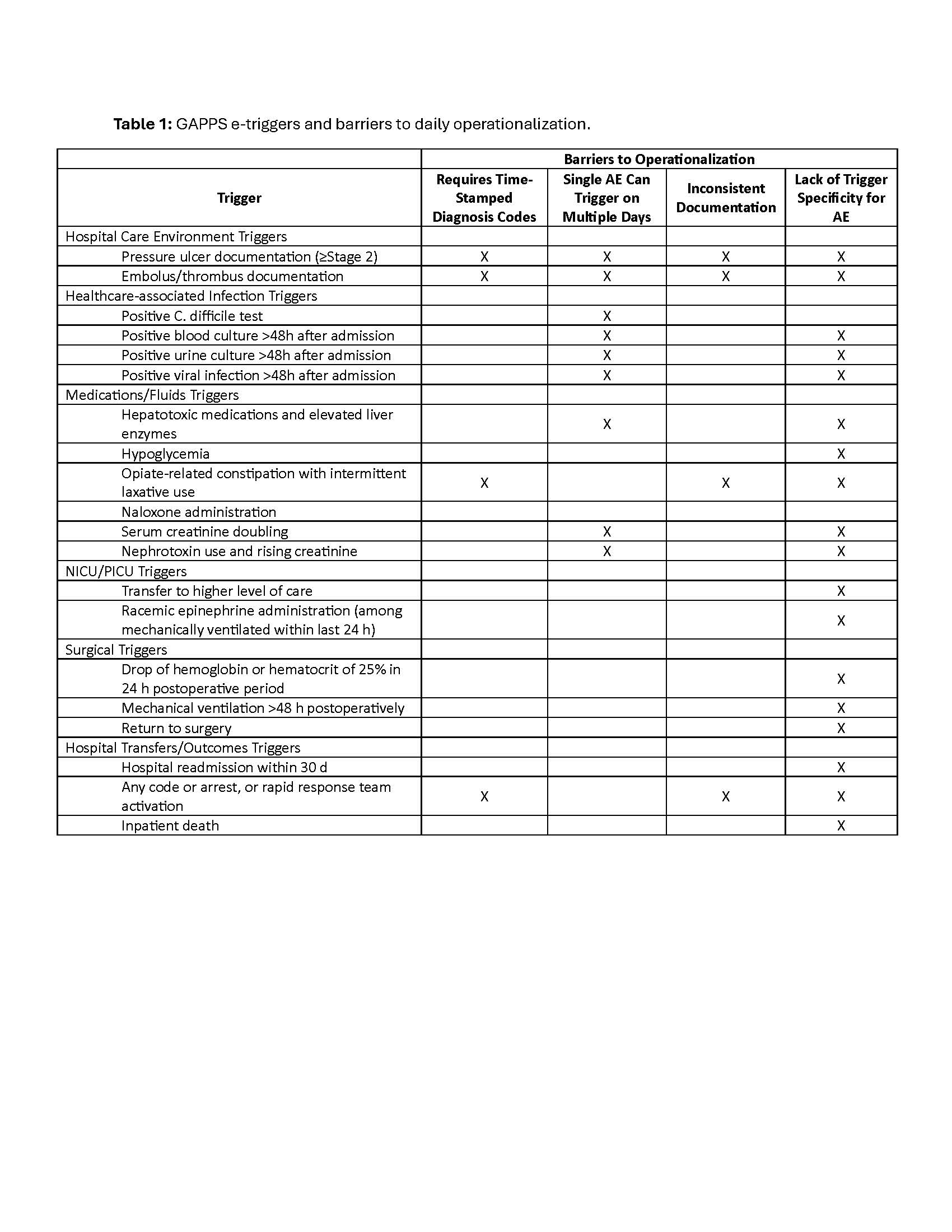
Figure 1: Prototype dashboard of monthly e-trigger rate for 20 triggers (demonstration data only).
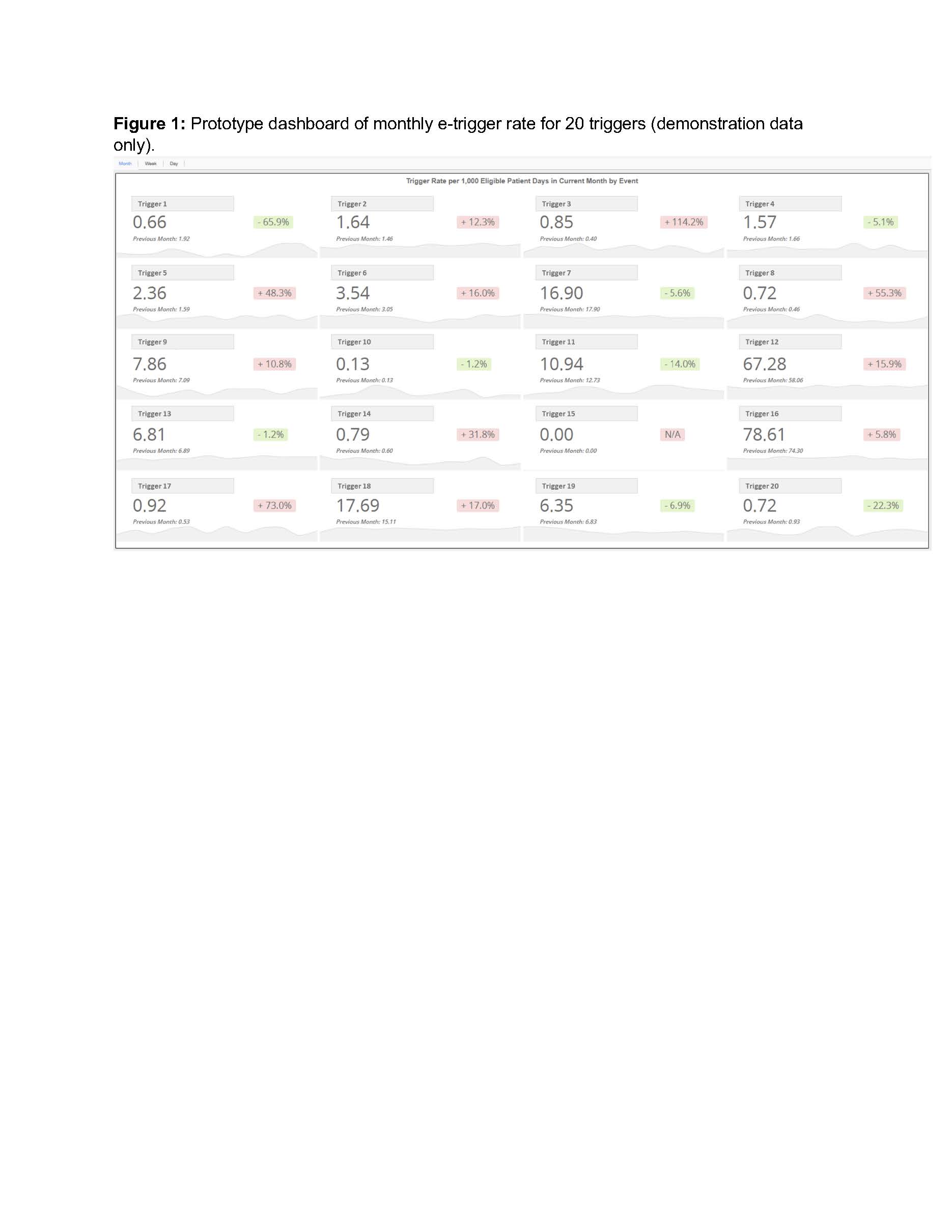
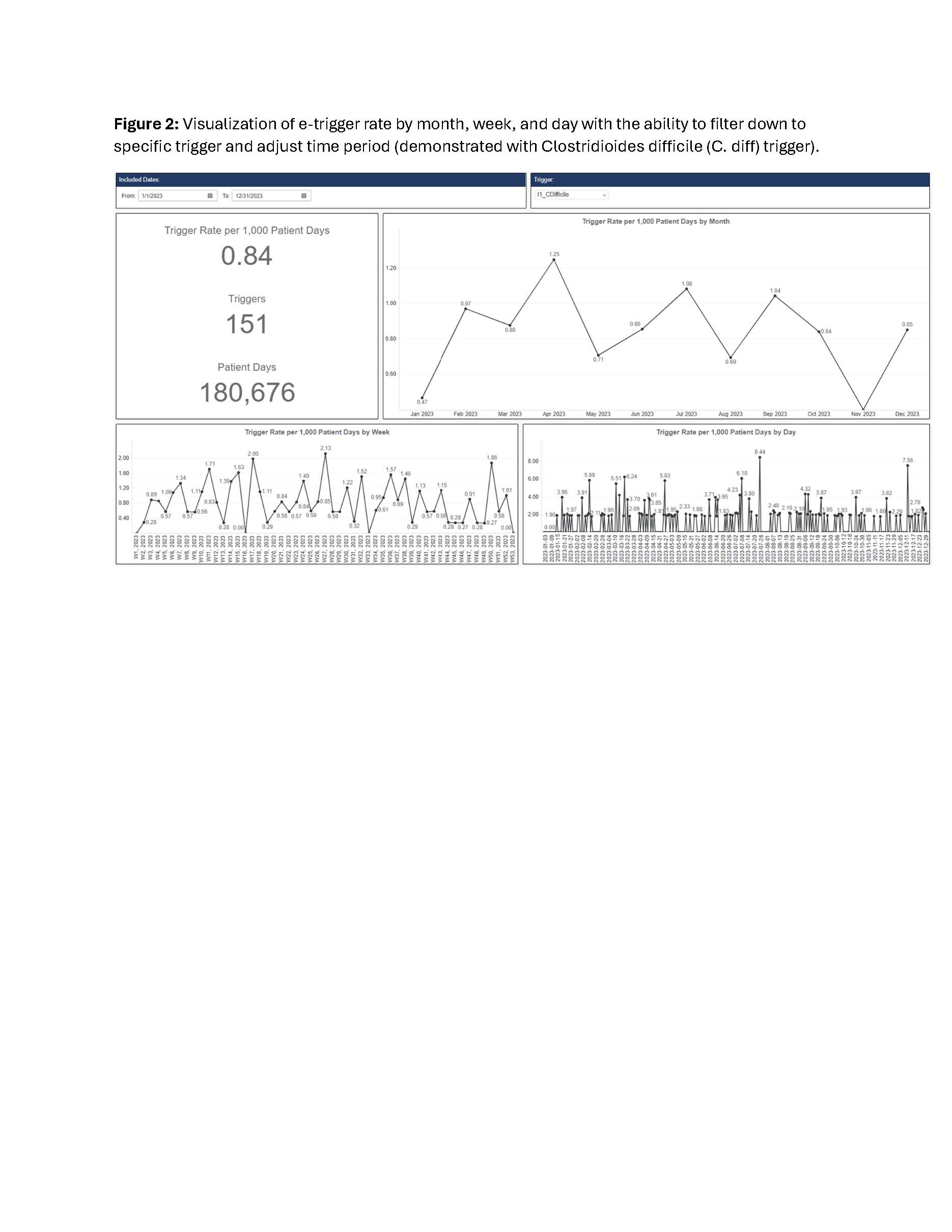
Figure 2: Visualization of e-trigger rate by month, week, and day with the ability to filter down to specific trigger and adjust time period (demonstrated with Clostridioides difficile (C. diff) trigger).