Neonatal General 1: Respiratory, BPD
Session: Neonatal General 1: Respiratory, BPD
265 - ARG1 Expression as a Potential Biomarker for BPD Risk in Preterm Neonates
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 265.4013
Zainab Manan, University of Texas Medical Branch School of Medicine, Galveston, TX, United States; Alvaro Moreira, The University of Texas Health Science Center at San Antonio Joe R. and Teresa Lozano Long School of Medicine, San Antonio, TX, United States; Sunil Jain, University of Texas Medical Branch School of Medicine, Galveston, TX, United States
- SJ
Sunil Jain, MD (he/him/his)
University of Texas Medical Branch School of Medicine
Galveston, Texas, United States
Presenting Author(s)
Background: Bronchopulmonary dysplasia (BPD) is a prevalent and severe respiratory complication in preterm neonates, particularly those with extremely low gestational age (ELGA). Emerging evidence suggests that arginine metabolism, integral to nitric oxide synthesis and immune function, may influence BPD pathogenesis. ARG1 (arginase 1), a key enzyme in this pathway, has the potential as a biomarker to identify neonates at high risk for BPD.
Objective: To evaluate the association of ARG1 expression with gestational age (GA) and BPD and to assess the predictive potential of ARG1 for BPD.
Design/Methods: This secondary analysis used publicly available whole-blood microarray data from 97 VLBW neonates in Poland (NCBI, 2011). Samples were collected on day of life 5, with ARG1 expression log2-transformed and quantile-normalized. BPD was defined per NICHD criteria. Analyses included: (1) linear regression to examine ARG1 expression relative to GA, (2) stratified analysis of ARG1 by GA group (extremely preterm, GA < 28 weeks; very preterm, GA 28–32 weeks), (3) comparison of ARG1 expression by BPD status within GA strata, and (4) ROC analysis to assess the predictive value of ARG1 for BPD.
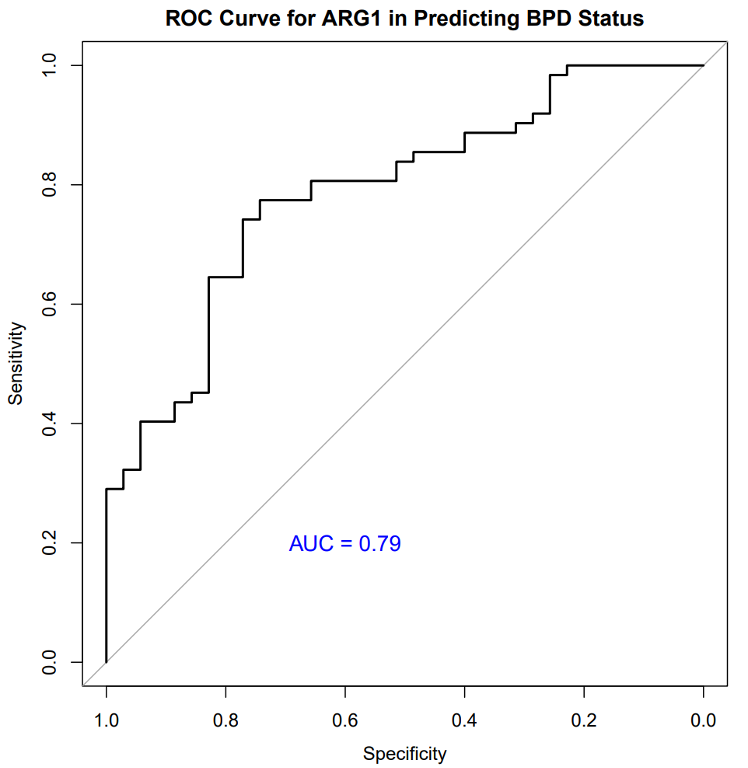
Results: Neonates who developed BPD had significantly lower GA (median 26.0 vs. 30.0 weeks) and birth weight (median 800 vs. 1,280 g) compared to those without BPD. ARG1 expression was inversely correlated with GA (r = -0.55, p < 0.001), with elevated ARG1 levels in younger gestational ages. In the extremely preterm group, ARG1 expression was significantly associated with BPD (p = 0.02). ROC analysis yielded an area under the curve (AUC) of 0.79 for ARG1 as a BPD predictor. The optimal ARG1 threshold was 0.63, with 77.4% sensitivity and 74.3% specificity.
Conclusion(s): Our findings suggest that ARG1 expression is strongly associated with GA and significantly elevated in ELGA neonates who develop BPD. This association may reflect the critical role of ARG1-mediated pathways in lung and immune development among extremely preterm infants, who are more vulnerable due to physiological immaturity. The ROC analysis supports ARG1 as a potential predictive biomarker for BPD, with good sensitivity and specificity. These findings warrant further investigation into the role of ARG1 and arginine metabolism in BPD and suggest ARG1 as a promising biomarker for identifying neonates at high risk for BPD.
Figure 1
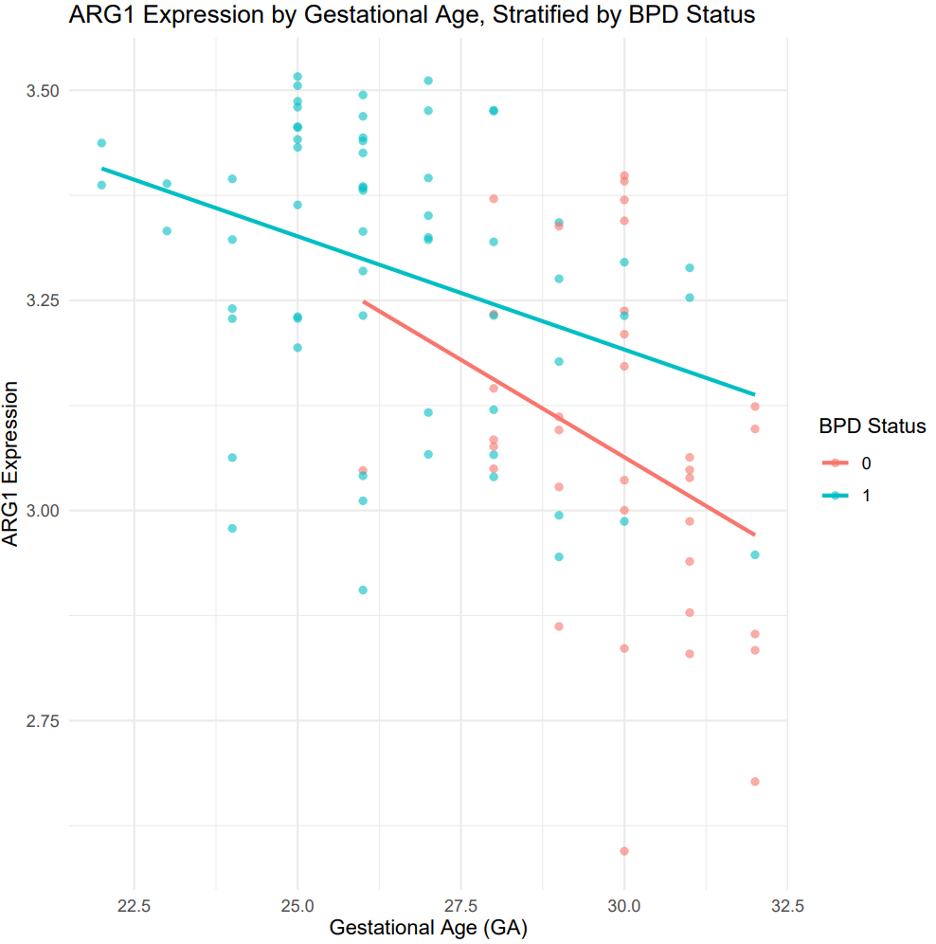
Figure 2
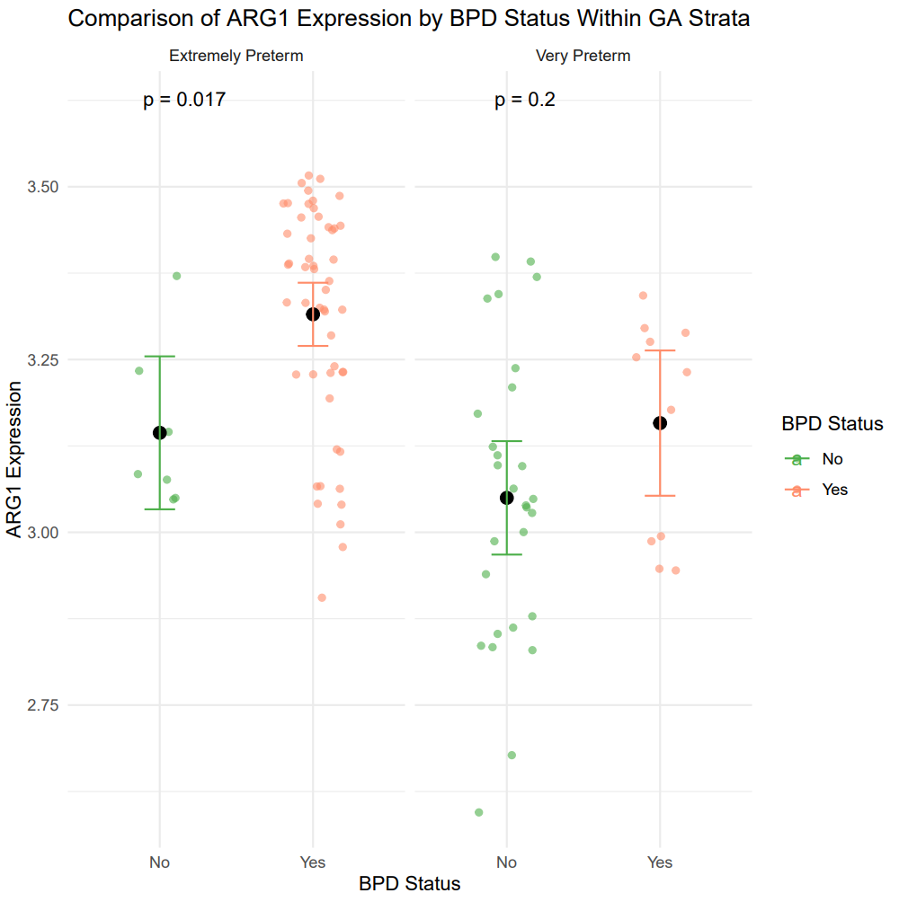
Figure 3