Neonatal/Infant Resuscitation 2
Session: Neonatal/Infant Resuscitation 2
305 - Cerebral Blood Flow Monitoring after Cardiopulmonary Resuscitation in Hypoxic Piglets using Diffuse Correlation Spectroscopy
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 305.4439
Randolph J. Sinahon, Drexel University, Tinton Falls, NJ, United States; Kurtulus Izzetoglu, Drexel University, Philadelphia, PA, United States; Shadi N. Malaeb, Drexel University College of Medicine, Philadelphia, PA, United States
.jpg)
Randolph J. Sinahon (he/him/his)
PhD Candidate
Drexel University
Tinton Falls, New Jersey, United States
Presenting Author(s)
Background: The goal of cardiopulmonary resuscitation (CPR) is to generate sufficient blood flow to the heart and brain after circulatory collapse until advanced care can be provided and the return of spontaneous circulation (ROSC) is achieved. Properly executed chest compressions (CC) pump blood from the heart to the vital organs, while shallow compressions lead to poor-quality CPR and worse outcomes. ROSC depends on the return of coronary perfusion. Anatomically, blood flow in the carotids indicates blood flow to the more proximally originated coronaries during CC. Thus, measures of cerebral blood flow (CBF) may inform CPR performance. Diffuse correlation spectroscopy (DCS) is a novel non-invasive optical technique that measures microcirculatory CBF. DCS calculates relative blood flow indices (rBFI) by detecting intensity fluctuations of scattered light from moving red blood cells in tissues.
Objective: To determine if DCS can detect changes in CBF during CPR and post-ROSC following hypoxia-induced circulatory collapse in piglets.
Design/Methods: Hypoxic shock and circulatory collapse were induced in ventilated piglets (3-5 days old; n=7) via stepwise reductions in FiO2 from 21% to 6% for 30-60 min until circulatory collapse, followed by immediate CPR with 100% FiO2 reoxygenation, chest compressions, with (n=4) and without (n=3) i.v. epinephrine. DCS probes applied to the head measured CBF via rBFI.
Results: Paired t-tests showed increased rBFI during CPR compared to pre-CPR (p=0.01), with and without epinephrine (Figure 1). Repeated measures ANOVA showed a large and significant effect of Condition (Baseline, Collapse/pre-CPR, post-ROSC) on rBFI and on heart rate (HR; p< 0.01; Figure 2). Post hoc tests showed rBFI decreased significantly from Baseline to Collapse/pre-CPR and increased post-ROSC, though still reduced compared to Baseline. HR decreased from Baseline to severe bradycardia/asystole during collapse/pre-CPR, but returned to sustained rates post-ROSC, indicating continued cerebral hypoperfusion despite achieving ROSC.
Conclusion(s): The results demonstrated that DCS measures of CBF matched expected changes in systemic perfusion after hypoxia-induced circulatory collapse, as well as during chest compression and post-ROSC. Often, chest compressions may be too shallow for size in the pediatric population, with many survivors experiencing ineffective resuscitation. Our findings suggest that DCS could serve as a non-invasive monitoring tool to guide CPR efforts and improve resuscitation outcomes.
Figure 1
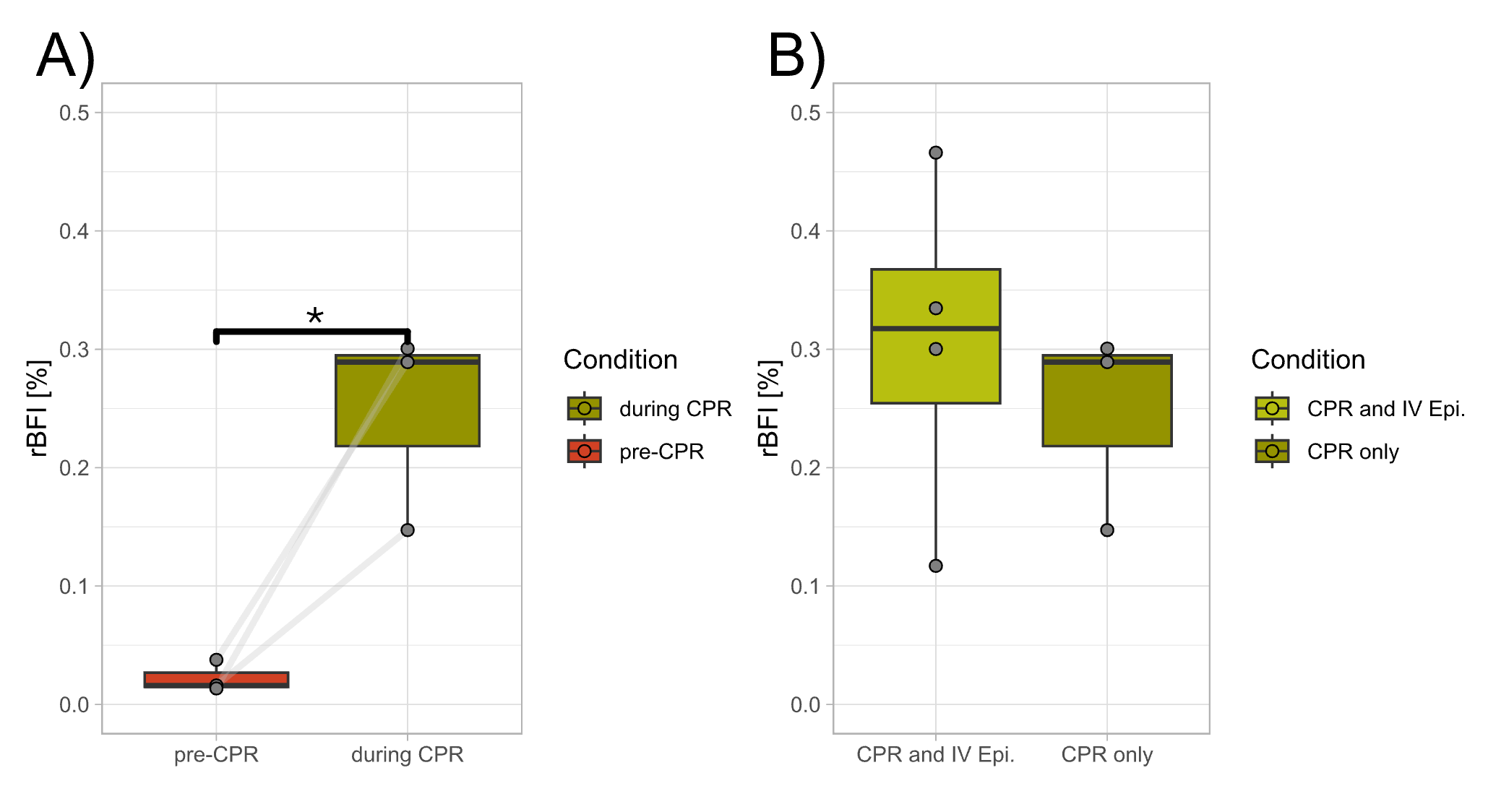 Figure 1: (A) Relative blood flow (rBFI) indices during circulatory collapse pre-CPR, and during CPR in piglets that did not receive initial intravenous epinephrine doses (n=3); Light gray lines represent individual animal responses (Two-tailed paired t- test; *p < 0.05, Hedges’ g=1.56). (B) rBFI during CPR with (n=3) and without (n=4) intravenous epinephrine (independent samples t-test; p= non-significant).
Figure 1: (A) Relative blood flow (rBFI) indices during circulatory collapse pre-CPR, and during CPR in piglets that did not receive initial intravenous epinephrine doses (n=3); Light gray lines represent individual animal responses (Two-tailed paired t- test; *p < 0.05, Hedges’ g=1.56). (B) rBFI during CPR with (n=3) and without (n=4) intravenous epinephrine (independent samples t-test; p= non-significant). Figure 2
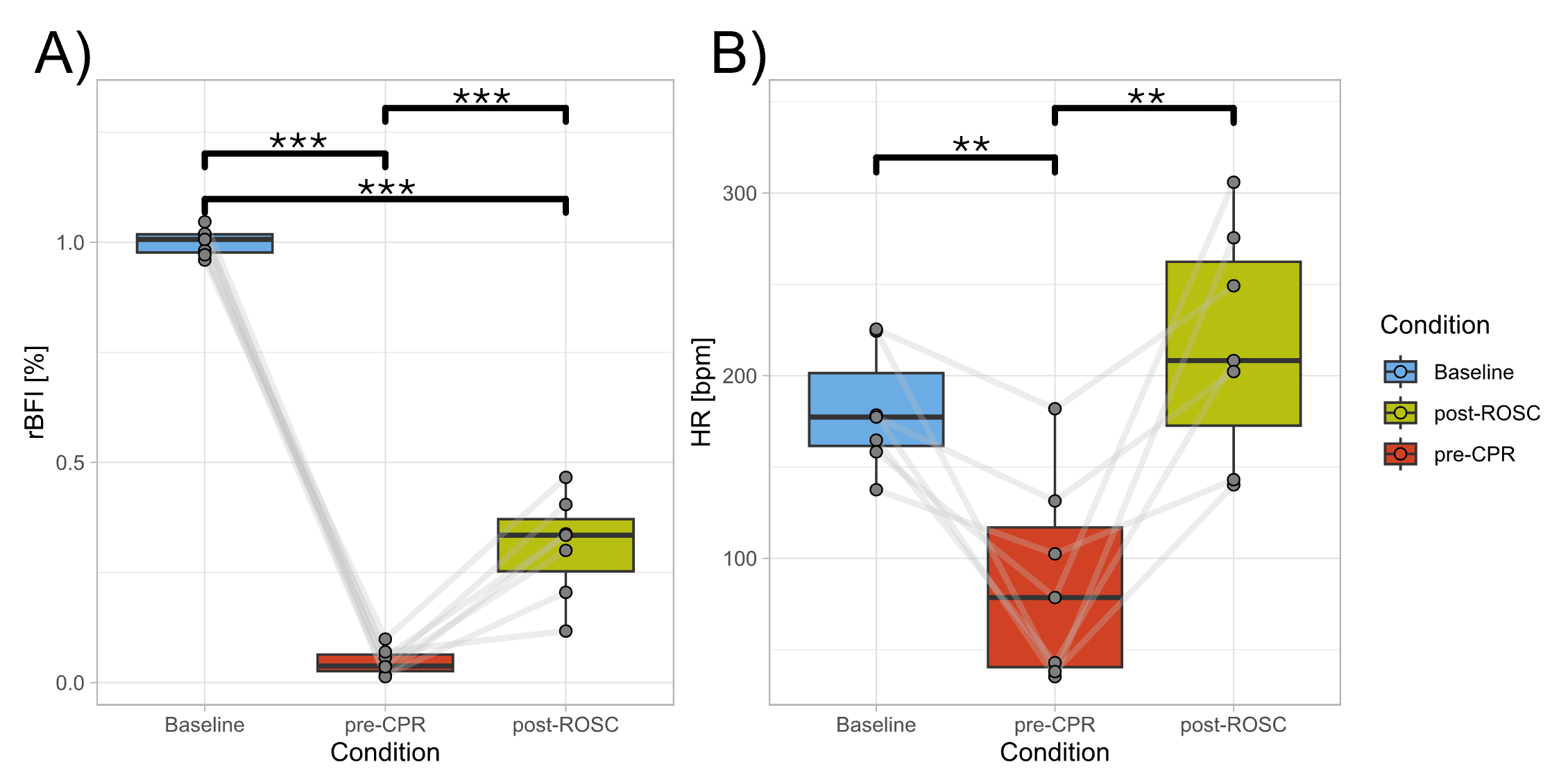 Figure 2: Repeated measures ANOVA and post hoc tests with false discovery rate corrections were used to compare (A) relative blood flow indices (rBFI; F(2,12)=349, ηp²=0.97) and (B) Heart Rate (HR; F(2,12)=13, ηp²=0.57) across Condition: Baseline, Circulatory Collapse/pre-CPR, and after Resuscitation/post-ROSC (n=7). Light gray lines represent individual animal responses (***p < 0.001, **p < 0.01). Hedges’ g effect sizes: rBFI Baseline v.s. pre-CPR (g=-16.3), pre-CPR v.s. post-ROSC (g= 2.01), and Baseline v.s. post-ROSC (g=-5.15); HR Baseline v.s. pre-CPR and pre-CPR v.s. post-ROSC (g=-1.40 and 1.41 respectively).
Figure 2: Repeated measures ANOVA and post hoc tests with false discovery rate corrections were used to compare (A) relative blood flow indices (rBFI; F(2,12)=349, ηp²=0.97) and (B) Heart Rate (HR; F(2,12)=13, ηp²=0.57) across Condition: Baseline, Circulatory Collapse/pre-CPR, and after Resuscitation/post-ROSC (n=7). Light gray lines represent individual animal responses (***p < 0.001, **p < 0.01). Hedges’ g effect sizes: rBFI Baseline v.s. pre-CPR (g=-16.3), pre-CPR v.s. post-ROSC (g= 2.01), and Baseline v.s. post-ROSC (g=-5.15); HR Baseline v.s. pre-CPR and pre-CPR v.s. post-ROSC (g=-1.40 and 1.41 respectively).
