Neonatal General 1: Respiratory, BPD
Session: Neonatal General 1: Respiratory, BPD
274 - Outcomes of infants receiving premedication during surfactant administration via Less Invasive Surfactant Administration and INtubation-SURfactant-Extubation
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 274.5958
Savanah Gallegos, Los Angeles General Medical Center, Agoura Hills, CA, United States; Japmeet Sandhu, Los Angeles General, Los Angeles, CA, United States; Sheryar Siddiqui, CHOC Children's Hospital of Orange County, Gold River, CA, United States; Emilio Feliz Sala, Keck School of Medicine of the University of Southern California, Los Angeles, CA, United States; Rangasamy Ramanathan, Cedars Sinai Guerin Children's, Cedars Sinai Medical Center, Los angeles, CA, United States; Manoj Biniwale, Cedars Sinai Medical Center, Los Angeles, CA, United States
- SG
Savanah Gallegos, DO
Resident Physician
Los Angeles General Medical Center
Agoura Hills, California, United States
Presenting Author(s)
Background: Two common techniques used for surfactant administration are the INtubation-SURfactant-Extubation (INSURE) method and Less Invasive Surfactant Administration (LISA). Atropine and Fentanyl are often used to prevent bradycardia and provide analgesia during these procedures, although these medications may lead to adverse consequences.
Objective: The purpose of this study was to compare the adverse events and outcomes among infants receiving premedication (atropine or fentanyl) compared to no medications during surfactant administration with INSURE or LISA.
Design/Methods: This is a retrospective (2016 -2023) cohort study of neonates who received surfactant administration through either INSURE or LISA. Data was collected from the NICU database and electronic health records and analyzed using SPSS version 29.
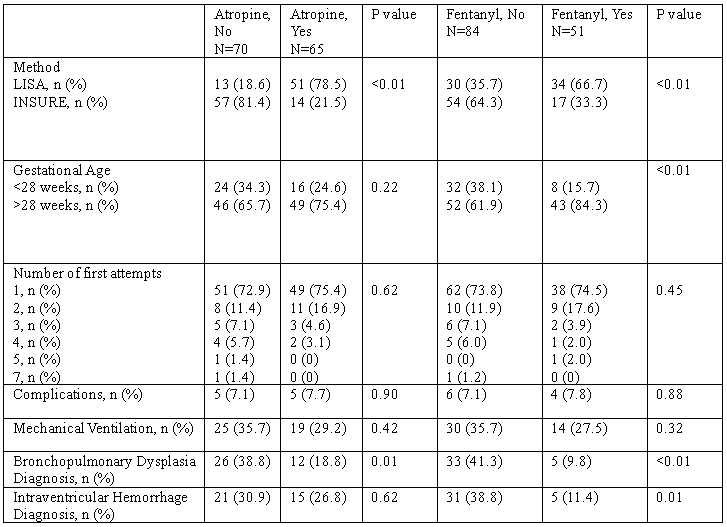
Results: Out of 135 infants, 53% received surfactant via INSURE; 47% received surfactant via LISA. 52% received atropine, 62% received fentanyl and 29% received both atropine and fentanyl. Infants receiving surfactant via LISA compared to INSURE were more likely premedicated with either atropine (p < 0.01) or fentanyl (p < 0.01). Of those receiving surfactant via LISA, 77% received both atropine and fentanyl. In infants who received premedication, a higher percentage of infants born >28 weeks gestational age only received fentanyl (p < 0.01). The number of first attempt procedures and rates of complications were similar in both groups. The percentage of infants requiring mechanical ventilation after receiving fentanyl, atropine, or no premedication with surfactant administration was not significantly different. Rates of intraventricular hemorrhage (IVH) diagnosis in patients who received fentanyl were lower compared to no sedation (11.4% vs 38.8%, p=0.01). Reduction of IVH was significant in patients who received sedation in the LISA group but not in the INSURE group. Bronchopulmonary dysplasia (BPD) was observed in a higher number of infants who did not receive atropine (p=0.01) and who did not receive fentanyl (p < 0.01). Regression analyses comparing infants who received premedication to those who did not revealed significant factors to be surfactant administration via LISA (p < 0.01) and decreased incidence of IVH (p=0.03).
Conclusion(s): Infants receiving surfactant via LISA and who were >28 weeks gestational age were more likely to receive premedication. Attempts and complications were not significantly different for infants receiving sedation versus no sedation. Infants who received atropine or fentanyl had significantly less BPD diagnoses; those who received fentanyl had a significantly lower rate of IVH.
Table 1: Outcomes of infants receiving premedication with atropine or fentanyl