Neonatal General 1: Respiratory, BPD
Session: Neonatal General 1: Respiratory, BPD
277 - Standardized Protocol for Caffeine Discontinuation in Extremely Preterm Infants: Impact on Practices, Cardiorespiratory Events, and Respiratory and Feeding Outcomes.
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 277.6726
Tiffany Mathieu, McGill University Health Centre, Dollard-Des-Ormeaux, PQ, Canada; Karina Paliotti, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada; Ramez Samy Helmy. Hanna, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada; Shasha Lv, McGill University Health Center, Montreal, PQ, Canada; Elissa Remmer, Montreal Children's Hospital, McGill University Health Center, Montreal, PQ, Canada; Francois Olivier, University McGill, Montréal, PQ, Canada; Aurore Cote, McGill University, Montreal, PQ, Canada; Guilherme Sant'Anna, McGill University Health Center, Montreal, PQ, Canada; Wissam Shalish, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada
- WS
Wissam Shalish, MD, PhD
Neonatologist
McGill University Health Center
Montreal, Quebec, Canada
Presenting Author(s)
Background: Caffeine is routinely administered to extremely preterm infants for cardiorespiratory events (CREs), but timing of discontinuation varies. Between 2019-2021, a protocol standardizing the timing of caffeine discontinuation was implemented at the Montreal Children’s Hospital (MCH) neonatal intensive care unit (NICU) (Fig 1).
Objective: To evaluate the protocol’s impact on 1) caffeine discontinuation and resumption practices; 2) clinically significant CREs; 3) respiratory and feeding outcomes.
Design/Methods: A retrospective cohort study was conducted for infants born < 28 weeks' GA at the MCH NICU. The cohort was divided into 3 groups (pre-protocol (2016-2019), peri-protocol (2019-2021) and post-protocol (2022)). Daily data on CREs, respiratory support, supplemental O2, and markers of feeding tolerance were collected at day –5 to +5 of caffeine discontinuation, on caffeine resumption day (if applicable), and from 34+0 to 40+0 weeks PMA. Statistical comparisons between the 3 groups were performed using the F-test for variability, Fisher’s exact test or Chi-square test for categorical variables, and either Wilcoxon’s rank sum test or t-test for continuous variables, as appropriate.
Results: 271 infants were included (138 pre-, 99 peri- and 34 post-protocol) with similar GA and birth weight. Timing of caffeine discontinuation remained similar across groups (PMA 36.8-37.1 weeks); however, variability was reduced post-protocol (p < 0.01 post vs. pre-, p=0.02 post- vs peri-) without affecting resumption rates. The median sum of CREs between 34+0 and 40+0 weeks PMA was lower in the post- vs pre- protocol group (p=0.003), as was the sum across all PMA weeks (p < 0.05) (Fig 2). There was also a reduction in infants requiring supplemental O2 or non-invasive respiratory support (NRS) at 39 weeks PMA post- vs. pre- protocol (p = 0.006) with no impact on indicators of feeding intolerance (Table 1).
Conclusion(s): Implementation of a caffeine protocol was associated with reduced variability in timing of discontinuation, reduced frequency of CREs, and less supplemental O2 or NRS at 39 weeks PMA, without negatively impacting other outcomes. This highlights the importance of standardization of respiratory care protocols for reducing unnecessary practice variations and potentially improving outcomes.
Figure 1. Flow Diagram of the Caffeine Discontinuation Protocol.
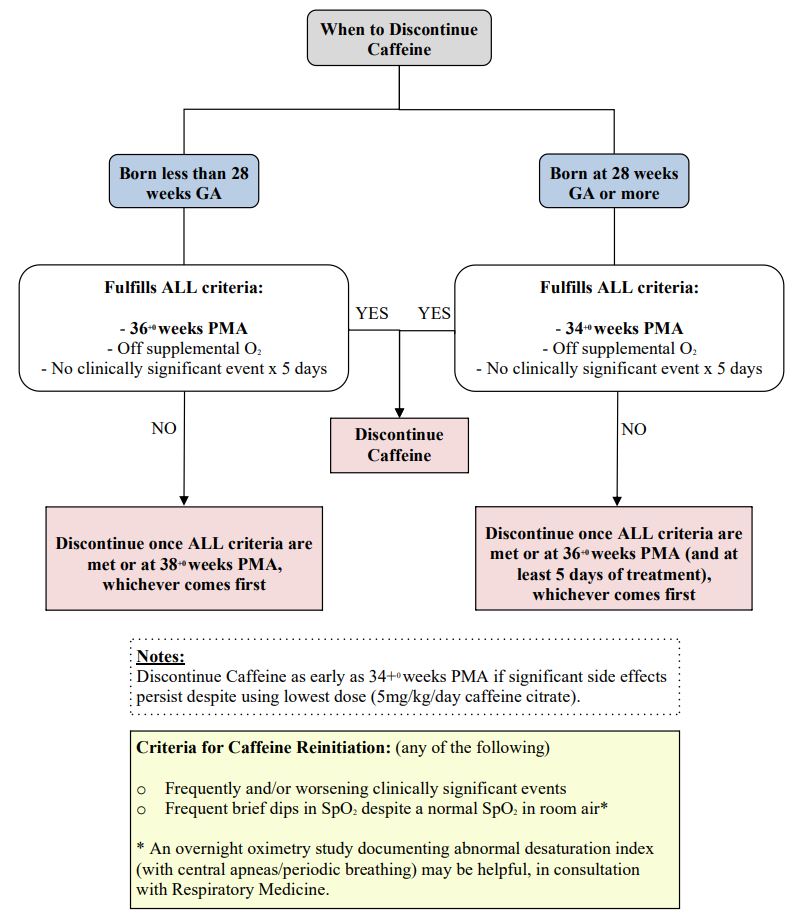
Figure 2. Comparing the sum of cardiorespiratory events per postmenstrual week.
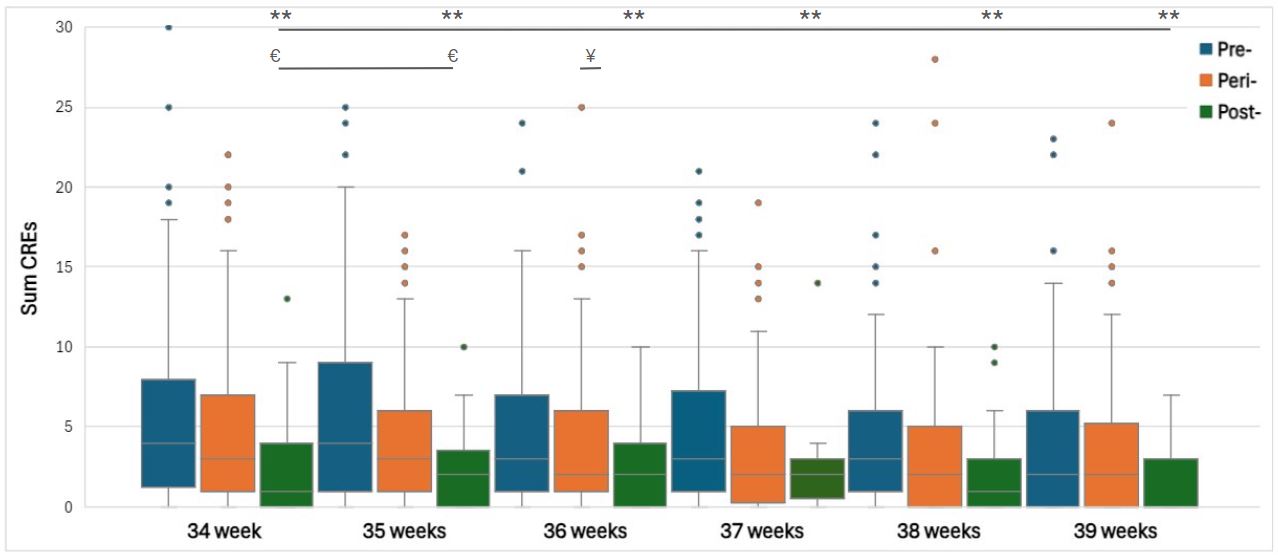 Legend: ¥; p <0.05 comparing pre- vs. peri-caffeine protocol, €; p <0.05 comparing peri- vs. post-caffeine protocol, **; p <0.05 comparing post- vs. pre-caffeine protocol. CREs (cardiorespiratory events) were defined as any nurse-recorded apneas, bradycardias, or desaturations requiring tactile stimulation, supplemental oxygen, and/or bag-mask ventilation.
Legend: ¥; p <0.05 comparing pre- vs. peri-caffeine protocol, €; p <0.05 comparing peri- vs. post-caffeine protocol, **; p <0.05 comparing post- vs. pre-caffeine protocol. CREs (cardiorespiratory events) were defined as any nurse-recorded apneas, bradycardias, or desaturations requiring tactile stimulation, supplemental oxygen, and/or bag-mask ventilation. Table 1. Respiratory and feeding outcomes pre-, peri-, and post- caffeine discontinuation protocol.
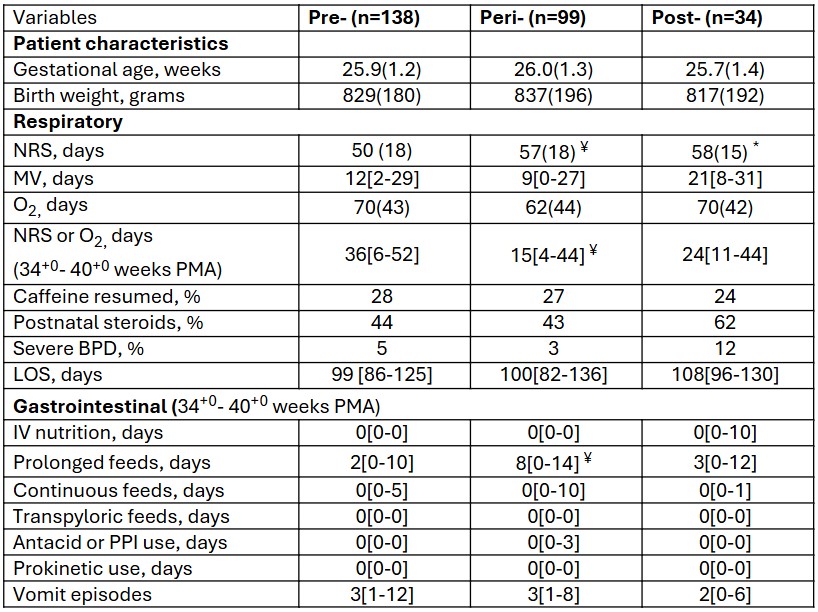 Abbreviations: BPD; bronchopulmonary dysplasia, LOS; length of stay, MV; mechanical ventilation, NRS; non-invasive respiratory support, O2; supplemental oxygen, PMA; postmenstrual age, PPI; proton pump inhibitor
Abbreviations: BPD; bronchopulmonary dysplasia, LOS; length of stay, MV; mechanical ventilation, NRS; non-invasive respiratory support, O2; supplemental oxygen, PMA; postmenstrual age, PPI; proton pump inhibitor Definitions: Prolonged feeds; feed duration >/= half of the feed frequency.
Analysis: Values are expressed as median [IQR], mean (SD), or percentage. ¥; p <0.05 for the comparison between pre- and peri- protocol, €; p <0.05 for the comparison between peri- and post- protocol, *; p <0.05 for the comparison between pre- and post- protocol.


