Immunizations/Delivery 1
Session: Immunizations/Delivery 1
674 - A novel, simulated, communication techniques training to address pediatric vaccine hesitancy in Japan and the Philippines
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 674.3837
Tatsuki Ikuse, Japan Pediatric Society, National Center for Child Health and Development, Setagayaku, Tokyo, Japan; Sarah Schaffer DeRoo, Children's National Hospital, Bethesda, MD, United States; Satoshi Kamidani, Emory University School of Medicine, Atlanta, GA, United States; Brande Brown, Boston Children's Hospital, Brooklyn, NY, United States; Akihiko Saitoh, Niigata University, Niigata, Niigata, Japan; Fatima I. Gimenez, Philippine Pediatric Society, Quezon City, Cavite, Philippines; Anelyn Logrono-Reyes, University of Santo Tomas, Philipppines, Las Pinas City, National Capital Region, Philippines; Angelina C. Bernardo, Philippine Pediatric Society, Pasig, National Capital Region, Philippines; Jehan Roselle C.. Santos, Philippine Pediatric Society, Pasig, National Capital Region, Philippines; Hannah Foehringer Merchant, American Academy of Pediatrics, Itasca, IL, United States; Kathryn Lander, American Academy of Pediatrics, Itasca, IL, United States; Aisha A. Tepede, American Academy of Pediatrics, Chicago, IL, United States; Mary Claire Eyre, American Academy of Pediatrics, Chicago, IL, United States; Samreen Vora, Yale School of Medicine, New Haven, CT, United States

Tatsuki Ikuse, MD, PhD (he/him/his)
Fellow
Japan Pediatric Society, National Center for Child Health and Development
Setagayaku, Tokyo, Japan
Presenting Author(s)
Background: Though immunization prevents 3-5 million deaths annually, vaccine hesitancy remains an obstacle to pediatric vaccine uptake. Presumptive communication and motivational interviewing (MI) are evidence-based physician-patient communication techniques for addressing vaccine hesitancy. Yet, little is known about their application in settings outside the United States.
Objective: We aimed to implement and evaluate a simulation-based workshop with pediatricians in Japan and the Philippines to assess physician perspectives on the application of these communication techniques in a global context.
Design/Methods: We developed a novel, simulation-based curriculum for pediatric vaccinators in these communication techniques. Key components of the curriculum included: 1) didactic instruction in presumptive communication and MI, and 2) simulation training in these skills via interactions with pre-recorded, video-based standardized participants. We trained physician facilitators from the Japan and Philippines Pediatric Societies in this curriculum, who then led 8-hour trainings with pediatric vaccinators in their respective countries. More details can be seen in Images 1-2. From January 2023 to April 2024, 120 vaccinators from Japan and 168 from the Philippines participated.
Results: 67 (56%) participants in Japan and 128 (76%) in the Philippines completed the first longitudinal survey after training participation. Detailed results are presented in Table 1. Among respondents in both countries, 84.6% felt extremely or very confident addressing vaccine hesitancy. Reported frequency of use and availability to utilize time varied across both countries. However, when asked if they experience more positive interactions with families around vaccine discussions after employing these communication techniques, 88% of respondents in Japan and 99% in the Philippines agreed or strongly agreed. Additionally, 73% of respondents in Japan and 98% in the Philippines agreed or strongly agreed when using the skills more families accept recommended vaccines.
Conclusion(s): Pediatric vaccinators in Japan and the Philippines reported high levels of confidence in addressing vaccine hesitancy and high perceived impact of skills on patient outcomes after participation in a training. Differences between countries may be attributable to differences in time spent with patients, physician comfort level with the techniques, and the cultural context. Further investigation of longitudinal use and perception of skills after the training is ongoing.
Image 1: Video-based simulated patient cases
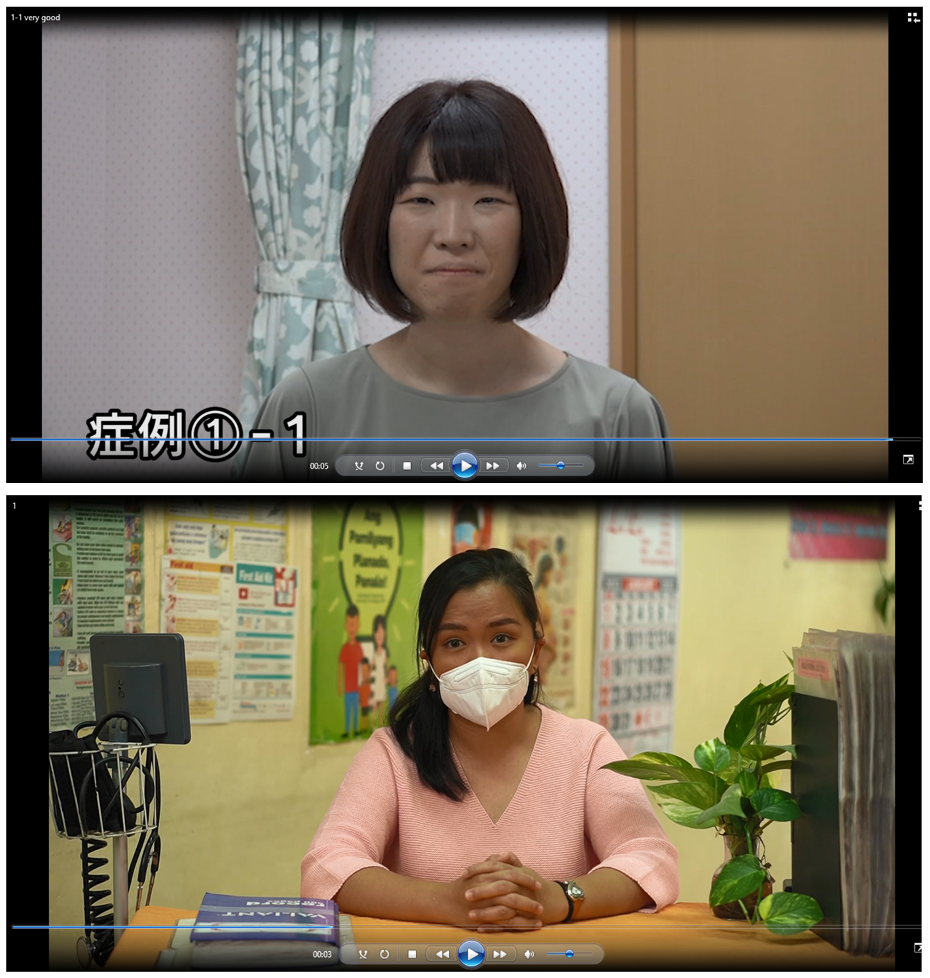 Simulation case presenting a vaccine conversation video developed and produced by the Japan Pediatric Society (top) and the Philippine Pediatric Society (bottom). Training facilitators navigated through the case using predetermined conversation pathways using Annenberg Hotkeys to modify the virtual patient’s response based on the training participant’s vaccine counseling. Japanese actors portrayed parents of pediatric patients and communicated in Japanese, and Filipino actors portrayed parents of pediatric patients and communicated in English.
Simulation case presenting a vaccine conversation video developed and produced by the Japan Pediatric Society (top) and the Philippine Pediatric Society (bottom). Training facilitators navigated through the case using predetermined conversation pathways using Annenberg Hotkeys to modify the virtual patient’s response based on the training participant’s vaccine counseling. Japanese actors portrayed parents of pediatric patients and communicated in Japanese, and Filipino actors portrayed parents of pediatric patients and communicated in English.Image 2: Facilitator guides for simulation navigation
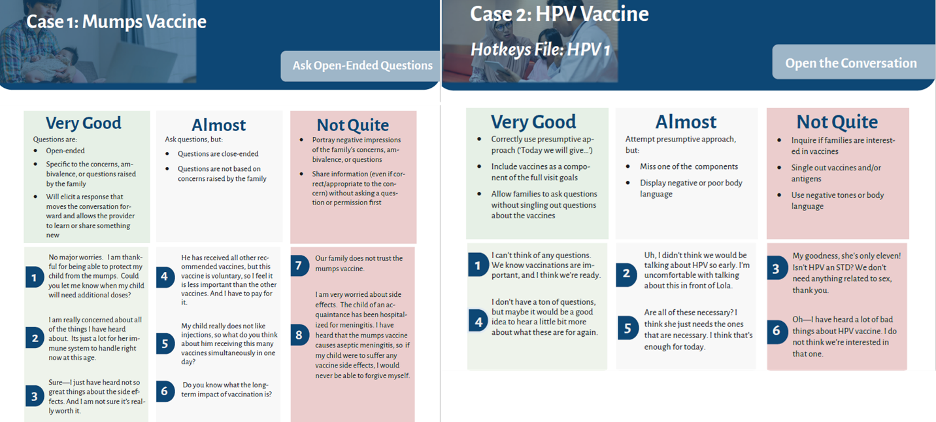 Hotkeys navigation for the training facilitator used to adapt the virtual patient’s responses to the training participant’s vaccine counseling. In these examples, participants practiced presumptive communication (left) and explored vaccine hesitancy by asking open-ended questions (right). In response to the participant’s use of this communication technique, the training facilitator selected the virtual patient’s response. The facilitator guide was developed in both English and Japanese in Japan and in English in the Philippines.
Hotkeys navigation for the training facilitator used to adapt the virtual patient’s responses to the training participant’s vaccine counseling. In these examples, participants practiced presumptive communication (left) and explored vaccine hesitancy by asking open-ended questions (right). In response to the participant’s use of this communication technique, the training facilitator selected the virtual patient’s response. The facilitator guide was developed in both English and Japanese in Japan and in English in the Philippines. Table 1: Results of post-training survey
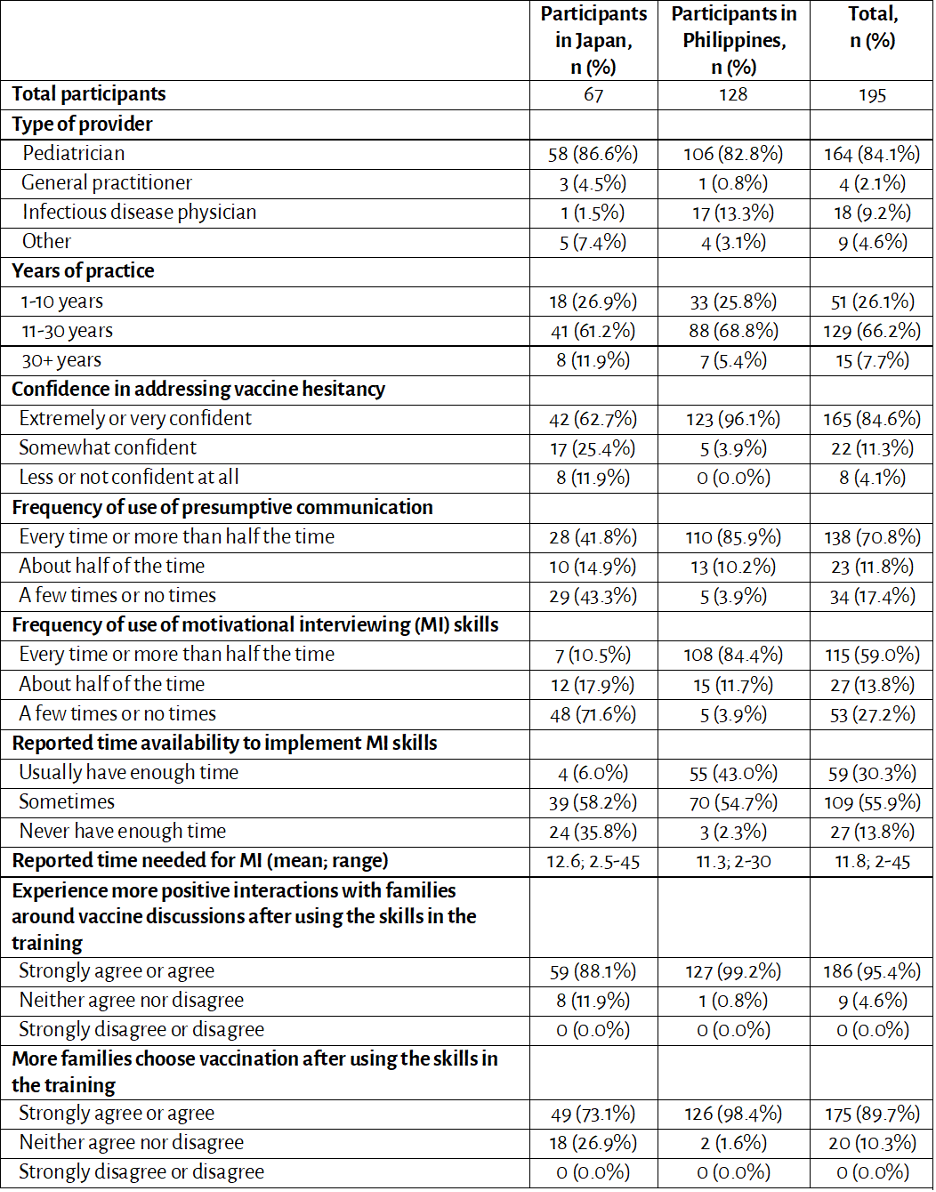 Summarized results from the first post-training survey conducted in Japan and Philippines after participating in the training in 2023-2024.
Summarized results from the first post-training survey conducted in Japan and Philippines after participating in the training in 2023-2024.
