Neonatal Neurology 2
Session: Neonatal Neurology 2
356 - Brain Injury and Neurodevelopmental Outcomes of Neonates with Congenital Heart Disease Born Preterm versus Term
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 356.4280
Aranni Prathepan, The Hospital for Sick Children, Toronto, ON, Canada; Vanna Kazazian, The Hospital for Sick Children, Toronto, ON, Canada; Stephanie Au-Young, The Hospital for Sick Children, Toronto, ON, Canada; Vann Chau, The Hospital for Sick Children, Toronto, ON, Canada; Ting Guo, The Hospital for Sick Children, Toronto, ON, Canada; Amandeep Kaur. Saini, The Hospital for Sick Children, Brampton, ON, Canada; Linh G. Ly, University of Toronto Temerty Faculty of Medicine, Toronto, ON, Canada; Helen Branson, The Hospital for Sick Children, Toronto, ON, Canada; Thiviya Selvanathan, University of British Columbia Faculty of Medicine, vancouver, BC, Canada; Mike Seed, University of Toronto, Toronto, Ontario/Canada, ON, Canada; Steven Miller, University of British Columbia Faculty of Medicine, Vancouver, BC, Canada

Aranni Prathepan, BScN, RN
Registered Nurse
The Hospital for Sick Children
Toronto, Ontario, Canada
Presenting Author(s)
Background: The effects of prematurity on neurodevelopment in neonates with cyanotic congenital heart disease (cCHD) is currently not well understood.
Objective: This study aimed to explore the neurologic and neurodevelopmental differences between neonates with cCHD born preterm and those born at term.
Design/Methods: A retrospective cohort of preterm neonates with cCHD born < 37 weeks gestational age (GA) between March 2016- December 2020 was compared to a prospective cohort of term neonates with single ventricle physiology (SVP) and transposition of the great arteries (TGA) born >36 weeks GA between May 2016-March 2020 at a single quaternary pediatric cardiac centre. Brain magnetic resonance imaging (MRI) was performed pre- and/or post-operatively for clinical and research indications on a 1.5T Avanto or 3T Siemens Prisma scanner. Neurodevelopmental outcomes were evaluated at 18 months corrected GA using the Bayley-III Scales of Infant and Toddler Development.
Results: 98 preterm neonates with cCHD (median GA 34.6 weeks; IQR 32-36) and 113 term neonates with SVP (48%, n=54) and TGA (52%, n=59) (median GA 39 weeks; IQR 38-40) were included. In the preterm cohort, 30% (n=29) of neonates had SVP and 10% (n=10) of neonates had TGA. Neonates in the preterm cohort were more likely to need extracorporeal membrane oxygenation (ECMO) during their hospital stay (p=0.03) and had a higher likelihood of dying in the neonatal period (p=0.001; Table 1).
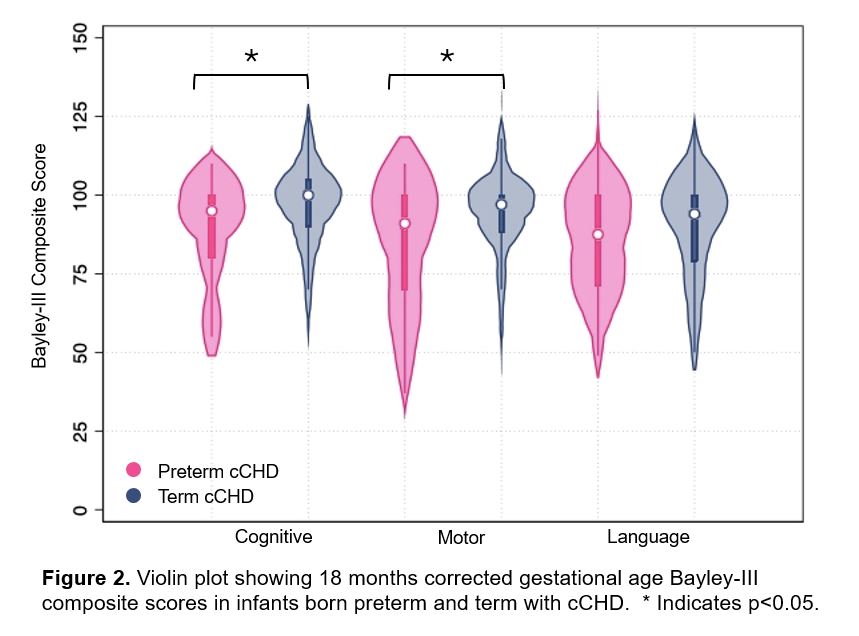
Neonates in the preterm cohort had more severe brain injury measured with Brain Injury Severity Score (BISS) than those in the term cohort (pre-op p< 0.001; post-op p=0.009) (Figure 1A). Neonates born preterm with cCHD were more likely to have pre-operative white matter injury (WMI) (p=0.01) that was more severe (p=0.001), and new severe WMI post-operatively compared to the term neonates (p=0.01; Figure 1B). There were no significant differences between the cohorts with regards to prevalence of stroke, cerebellar hemorrhage, intraventricular hemorrhage, or hypoxia ischemia pre- or post-operatively.
Neurodevelopmental outcomes at 18 months’ corrected GA revealed poorer cognitive (p=0.003) and motor (p=0.02) outcomes in the preterm cohort (Figure 2).
Conclusion(s): Neonates with cCHD born preterm face a distinct set of risks that impact the brain and neurodevelopmental outcomes when compared with term neonates with cCHD. Specifically, preterm neonates with cCHD are more vulnerable to moderate-severe WMI and are at increased risk for cognitive and motor delays.
Table 1
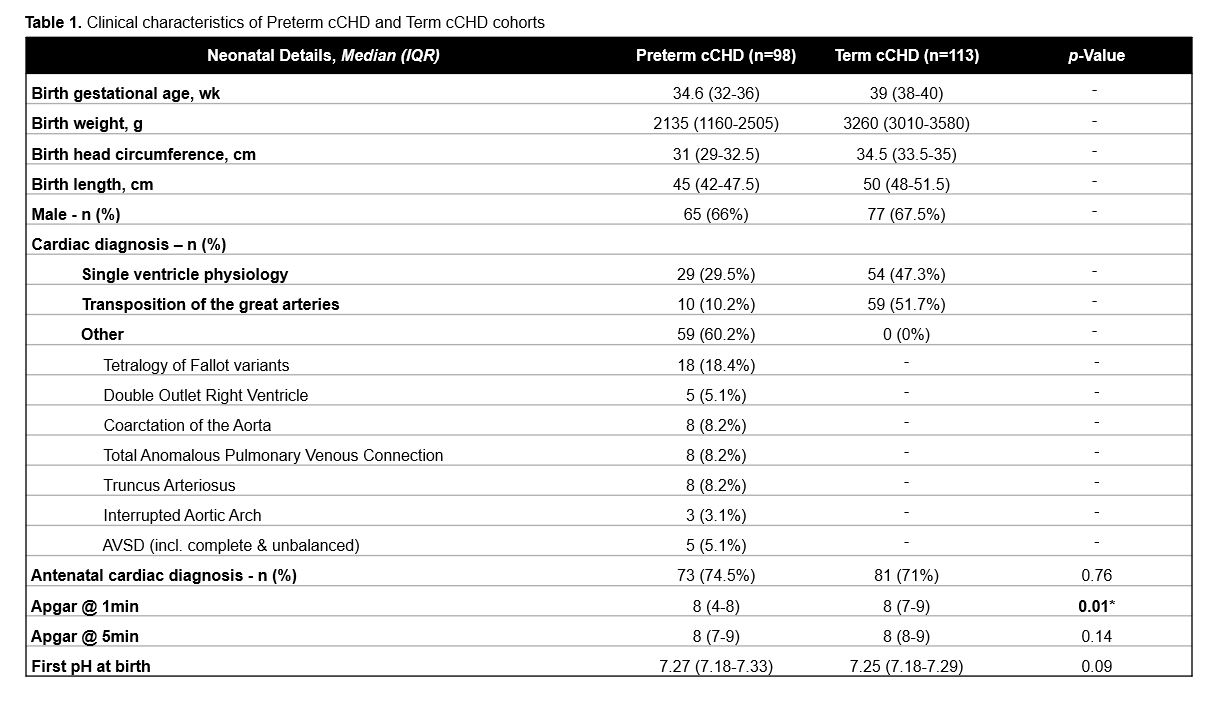
Figure 1
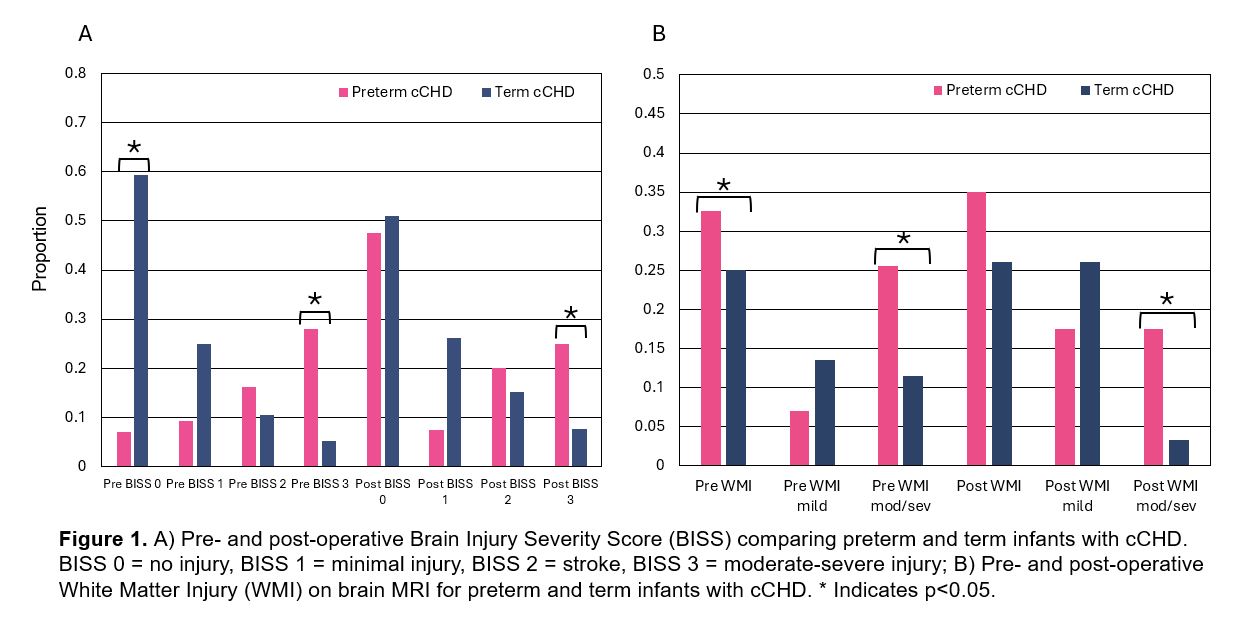
Figure 2