Neonatal Neurology 1
Session: Neonatal Neurology 1
343 - Punctate White Matter Injury in Moderate-to-Late Preterm Infants: Lesion Load, Spatial Distribution, and Comparison with Other Neonatal Populations
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 343.6412
Ting Guo, The Hospital for Sick Children, Toronto, ON, Canada; Eleanor Kennedy, University of Auckland, Auckland, Auckland, New Zealand; Sian A. Williams, University of Auckland, Auckland, Auckland, New Zealand; Thiviya Selvanathan, University of British Columbia Faculty of Medicine, vancouver, BC, Canada; Jane M. Alsweiler, School of Medicine, University of Auckland, Auckland, Auckland, New Zealand; Frank H. Bloomfield, University of Auckland, Auckland, Auckland, New Zealand; Malcolm Battin, Auckland City Hospitial, Auckland, Auckland, New Zealand; David Dubowitz, University of Auckland, Auckland, Auckland, New Zealand; Steven Miller, University of British Columbia Faculty of Medicine, Vancouver, BC, Canada; Catherine Morgan, University of Auckland, Auckland, Auckland, New Zealand; David H. Perry, Starship Children’s Health Te Toka Tumai Auckland, Auckland, Auckland, New Zealand; Ngaire Susan Stott, The University of Auckland, Grafton, Auckland, New Zealand; Jane E. Harding, Liggins Institute, University of Auckland, Auckland, New Zealand, Auckland, Auckland, New Zealand
- JG
Jessie Ting Guo, PhD
Senior Research Associate
The Hospital for Sick Children
Toronto, Ontario, Canada
Presenting Author(s)
Background: Over 80% of all preterm births occur in the moderate-to-late preterm (MLP) period (32 to 36 weeks’ gestation). MLP infants are at increased risk for neurodevelopmental impairments. White matter injury (WMI) is the characteristic brain injury in very preterm (VP) infants and predicts adverse outcomes. However, little is known about WMI in MLP infants.
Objective: We investigated the burden and distribution of WMI in MLP infants, and compared them with those in VP infants and term infants with congenital heart disease (CHD).
Design/Methods: We recruited 101 MLP infants (32 females [31.7%], median [IQR] gestational age [GA]: 33.9 [33.1-34.6] weeks) from a randomised trial of neonatal nutrition and a prospective observational cohort in New Zealand. Brain MRI scans were acquired early-life (N = 98, median post-menstrual age [PMA]: 35.6 [34.7-36.1] weeks) and at term-equivalent age (N = 87, median PMA: 40.3 [39.4-40.9] weeks). WMI burden was quantified. Total and regional WMI volumes, and percentage of total cerebral volume (TCV) were obtained. WMI spatial distribution was assessed using quantitative lesion mapping and compared with that in VP infants at early-life and term infants with CHD.
Results: Forty infants (39.6%) had WMI. From early-life to term, WMI became less visible or undetectable in 29/37 infants (78.4%) with WMI who had both scans (Table 1). WMI volume reduced 72.7±207.5 mm3. Pregnancy or neonatal characteristics were not significantly different between infants with and without WMI. Gestation, sex, PMA at MRI, and other clinical factors were not associated with WMI volume or percentage. WMI in MLP infants occurred predominantly in the posterior regions, followed by central and anterior regions (Fig 1). The trigonal regions and areas around temporal and occipital horns were more vulnerable. WMI volume in MLP infants (median: 21.5 [8.8-70.0] mm3) was similar to that in two cohorts of VP infants (median: 16.0 [6.8-45.1] mm3, 43.9 [21.4-296.2] mm3), but smaller than that in 86 term CHD infants (88.0 [42.0-217.3] mm3). Trigonal areas were vulnerable across neonatal populations. However, MLP and VP infants had more lesions in bilateral central white matter than term CHD infants whose WMI was more wide-spread and extended more anteriorly and posteriorly (Fig 2).
Conclusion(s): In MLP infants, WMI is much more common than previously reported, and occurs in a characteristic topology, which shares homologous regions across neonatal populations. WMI in MLP infants may be missed on term-equivalent age MRI; its relationship with outcomes warrants investigation.
Table 1. Quantitative Measurements of White Matter Injury on Early-life and Term-equivalent Age MRI Scans – in the subgroup of 37 infants with white matter injury who underwent MRI at both early-life and term-equivalent age time points.
.png)
Figure 1. Probabilistic Map of Maximum White Matter Injury Identified in 40 MLP Infants on Early-Life or Term-Equivalent Age MRI.
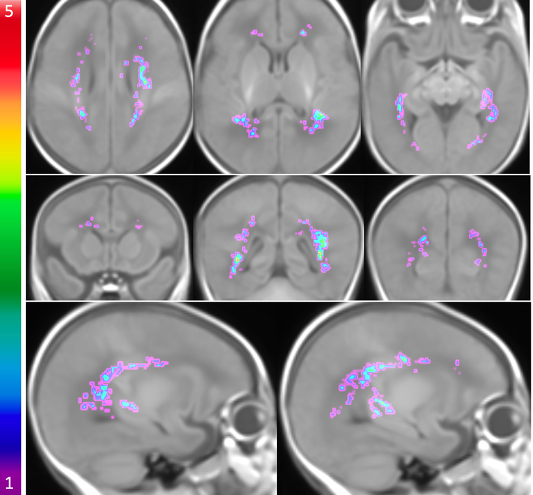 The probabilistic WMI map of 40 MLP infants overlaid on the brain template displayed on axial planes (superior to inferior), coronal planes (anterior to posterior), and sagittal planes (left to right). The colour bar on the left indicates the colour coding of the WMI summation where WMI occurs at homologous regions across the MLP infants.
The probabilistic WMI map of 40 MLP infants overlaid on the brain template displayed on axial planes (superior to inferior), coronal planes (anterior to posterior), and sagittal planes (left to right). The colour bar on the left indicates the colour coding of the WMI summation where WMI occurs at homologous regions across the MLP infants.Figure 2. Comparison of White Matter Injury Distribution between MLP Infants with Very Preterm Infants and Term CHD Infants.
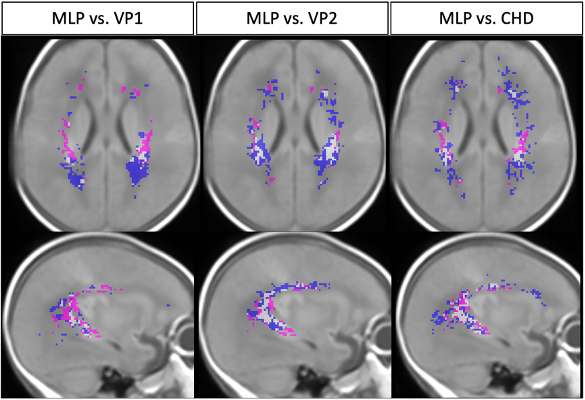 Comparison of WMI identified in 40 MLP infants at early-life or TEA with WMI in 68 very preterm infants from VP-cohort 1 (1st column) and in 58 very preterm infants from VP-cohort 2 (2nd column) at early-life, as well as with WMI in 86 term CHD infants (3rd column) on an axial plane and a sagittal plane of the brain template. Magenta: WMI identified only in MLP infants; Blue: WMI only in VP-cohort 1, VP-cohort 2 or CHD infants; White: WMI that are common in MLP and any other cohort.
Comparison of WMI identified in 40 MLP infants at early-life or TEA with WMI in 68 very preterm infants from VP-cohort 1 (1st column) and in 58 very preterm infants from VP-cohort 2 (2nd column) at early-life, as well as with WMI in 86 term CHD infants (3rd column) on an axial plane and a sagittal plane of the brain template. Magenta: WMI identified only in MLP infants; Blue: WMI only in VP-cohort 1, VP-cohort 2 or CHD infants; White: WMI that are common in MLP and any other cohort.
