Neonatal/Infant Resuscitation 1
Session: Neonatal/Infant Resuscitation 1
294 - Choosing the Primary Interface for Positive Pressure Ventilation in Neonatal Resuscitation: Preliminary Results of the Implementation of a Novel Supraglottic Airway Clinical Decision Support Tool
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 294.4081
Stephanie De Ocampo, Kaiser Foundation Hospital - Roseville Women's and Children's Services, Roseville, CA, United States; Patrick Motz, The Permanente Medical Group, Roseville, CA, United States; Carrie Ann Capansky, Kaiser Foundation Hospital - Roseville Women's and Children's Services, Roseville, CA, United States

Stephanie De Ocampo, MSN
Registered Nurse
Kaiser Foundation Hospital - Roseville Women's and Children's Services
Roseville, California, United States
Presenting Author(s)
Background: Our multidisciplinary Newborn Delivery Attendance Committee implemented recommendation 10 from the 2023 American Heart Association and American Academy of Pediatrics Focused Update on Neonatal Resuscitation. The update empowered the placement of a supraglottic airway (SA) as the primary interface (PI) for positive pressure ventilation (PPV) for newborn infants ≥34.0 weeks gestation but lacked specific guidance for the implementation of this change in practice.
Barriers to SA use in delivery room resuscitation (DRR) include inaccessibility of SA devices, inadequate training, limited clinical experience, lack of confidence in SA efficacy, and endotracheal tube preference. Providers also expressed concerns about potential device overuse, concerns that SAs are more invasive than face masks (FM), and uncertainty about which babies would most benefit from an SA as a PI for PPV.
Objective: We aim to address common barriers to SA use by implementing a novel SA clinical decision support tool (CDST).
Design/Methods: To address device safety concerns and provide guidance on SA use during DRR, we developed and implemented a novel SA CDST in conjunction with didactic and simulation training. The SA CDST is a simple algorithm that assists NRP providers to rapidly choose a PI to provide PPV in the delivery room. Our tool focuses on the assessment of tone to classify infants who need PPV as either Type I (some tone: PPV via FM as PI) or Type II (limp: PPV via SA as PI). We opted for tone as the key deciding indicator for the tool because the loss of tone is a late fetal physiologic sign of hypoxia, and the limp infant is likely severely depressed.
Results: In the first 60 days of the SA CDST implementation, with 1,070 recorded live births, there were (n=24) reported SA insertions. Of the 24 infants, 11 SAs were placed as PI, and 13 were placed as part of ventilation corrective steps (VCS). The median time an SA was in place was 115 seconds. There are no reported instances of airway trauma or death. SAs were placed by 12 registered nurses, 9 respiratory therapists, and 3 physicians. We also observed an increased use of the SA as part of VCS. Prior to the implementation of the SA CDST, less than 5 SAs were placed during DRR in the previous 5-year period. All SAs previous to this were placed exclusively by physicians.
Conclusion(s): Our preliminary data shows that implementation of the SA CDST equipped and safely guided NRP providers to choose a PI for PPV during DRR and significantly increased the use of SAs by non-physician NRP providers.
Supraglottic Airway Algorithm: Clinical Decision Support Tool
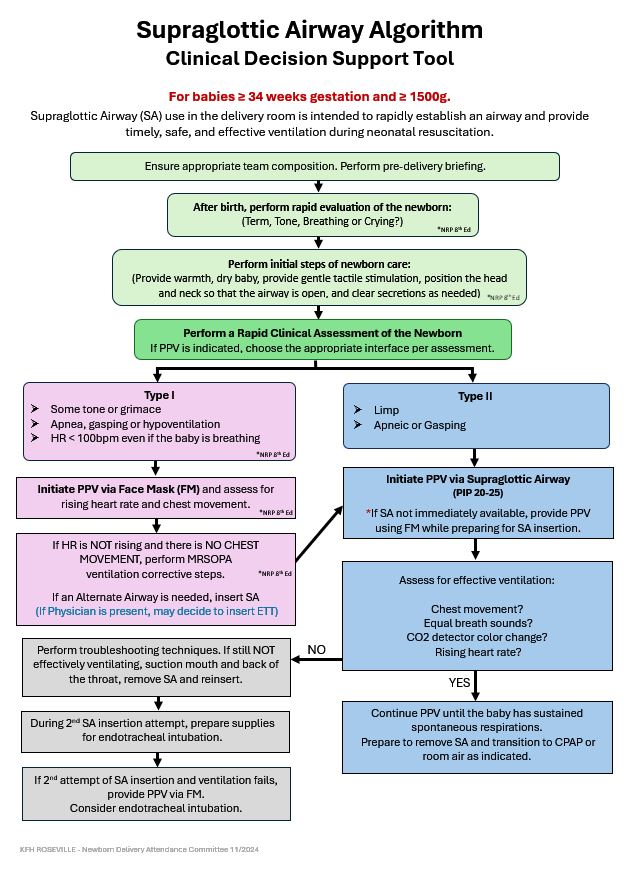 Figure 1: Supraglottic Airway Algorithm: Clinical Decision Support Tool
Figure 1: Supraglottic Airway Algorithm: Clinical Decision Support ToolSupraglottic Airway Preliminary Results Table
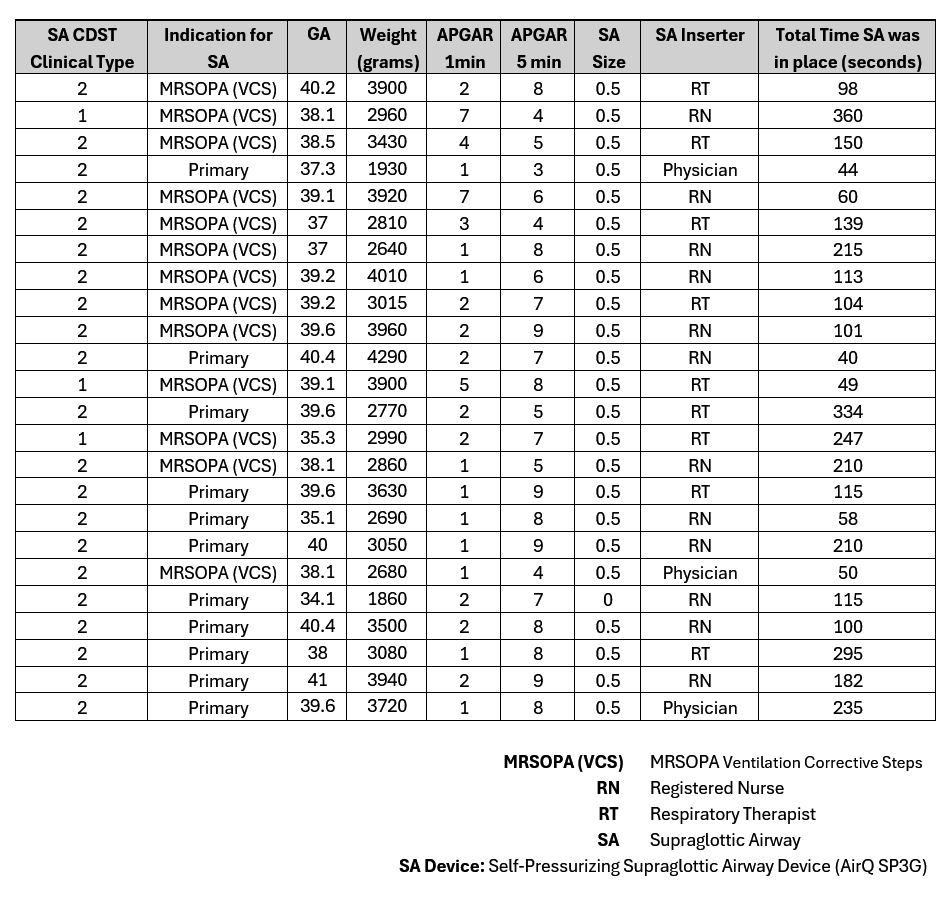 Table 1: Supraglottic Airway Insertion Report
Table 1: Supraglottic Airway Insertion ReportSA CDST Implementation Preliminary Results (60 Days)
Supraglottic Airway Algorithm: Clinical Decision Support Tool
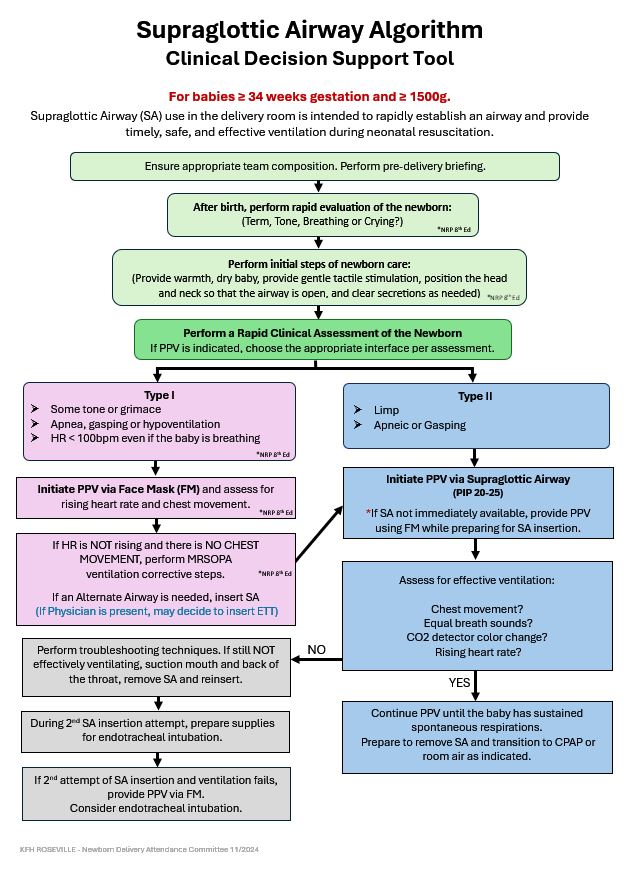 Figure 1: Supraglottic Airway Algorithm: Clinical Decision Support Tool
Figure 1: Supraglottic Airway Algorithm: Clinical Decision Support ToolSupraglottic Airway Preliminary Results Table
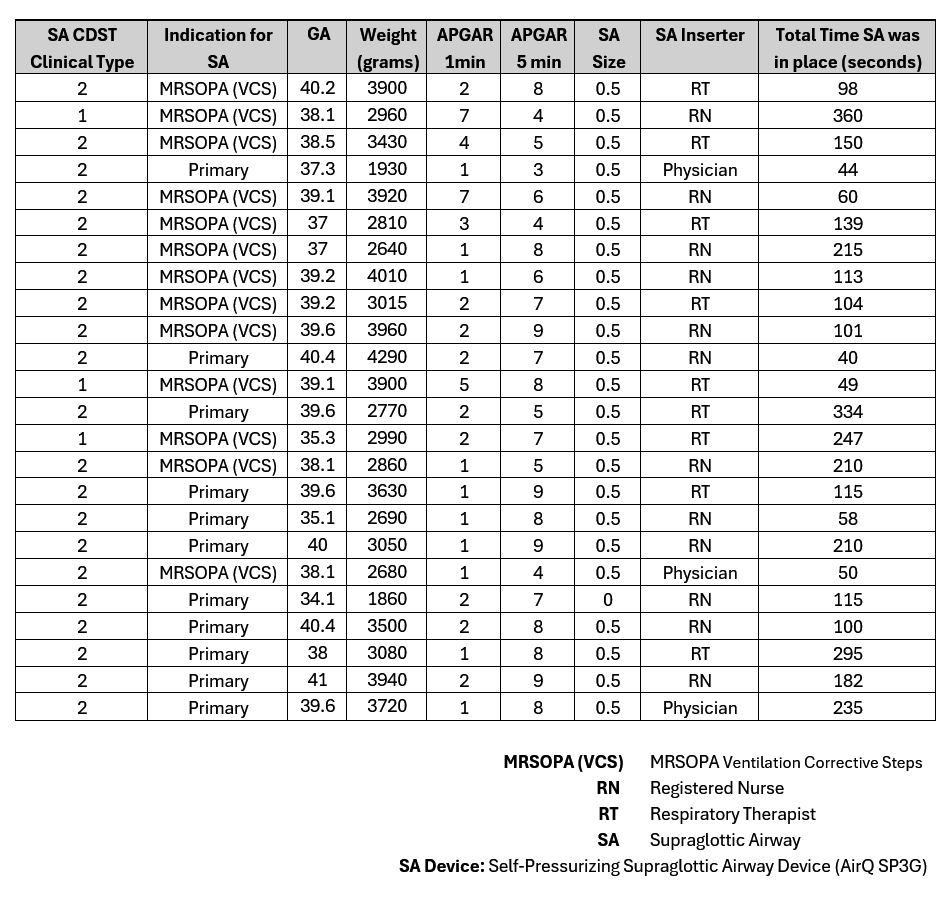 Table 1: Supraglottic Airway Insertion Report
Table 1: Supraglottic Airway Insertion ReportSA CDST Implementation Preliminary Results (60 Days)

