Neonatal General 3: NICU Practices
Session: Neonatal General 3: NICU Practices
557 - Infant Voice Exposure Through a Reading Program: Comparing Experiences in an Open Bay to a Single-Family Room NICU
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 557.5460
Malathi Balasundaram, Stanford University School of Medicine, Mountain View, CA, United States; Dharshi Sivakumar, Stanford University School of Medicine, Sunnyvale, CA, United States; Cody Arnold, Stanford University School of Medicine, Palo Alto, CA, United States

Malathi Balasundaram, MD (she/her/hers)
Clinical Professor
Stanford University School of Medicine
Mountain View, California, United States
Presenting Author(s)
Background: Single-Family Room (SFR) Neonatal Intensive Care Units (NICU) have shown benefits such as increased parental presence, enhanced parent−infant closeness and improved parental psychological well-being with reductions in parental depression and stress. Some studies showed the negative impacts of the SFR model were lower language scores and a strong trend toward worsening motor scores at 24-month follow-up. This could be due to the sensory isolation within the SFR environment if parental presence and engagement were low. We implemented a reading program in 2020 to provide critical vocal stimulation to NICU babies in our community Level III NICU with 4900 deliveries and 500 NICU admissions per year. In October 2023, we moved from a 20-bed open bay (OB) NICU to a 24-bed (SFR) NICU.
Objective: To compare average reading time per day (aveRM/d) for babies in the OB (January to October 2023) to SFR (November 2023 to June 2024), overall and aveRM/d by parents and aveRM/d by staff.
Design/Methods: Nurses and parents played a crucial role in this initiative, and their efforts were documented in the Electronic Health Record (EHR) (Figure 1). After one year in SFR we reviewed our reading program data to see if the new unit had an impact on the success of the program as measured by newborns’ aveRM/d. Reading time and covariate data was extracted from the EHR and aveRM/d was calculated by dividing each baby’s total reading minutes by the number of days in the NICU. Mean and median aveRM/d was compared with t-tests, linear regression and quantile regression respectively.
Results: There were 363 and 299 babies in the OB and SFM, respectively. Although gestational age (GA) and length of stay (LOS) were positively correlated with aveRM/d, mean/median GA and LOS were nearly identical between cohorts. [Table1] Figure 1 shows that mean aveRM/d was larger in the OB, for parents, staff, and overall. Adjusting for small differences in GA and LOS, the mean and median aveRM/d for OB versus SFM were 11 and 9 minutes versus 8 and 6 minutes, p-values < .001. (Table 1).
Conclusion(s): Our findings are consistent with previous studies suggesting decreased vocal exposure and potentially greater sensory isolation in a SFR. Potential causes are less focus on the reading program while staff adapted to the new SFR unit or increased workload for staff who are now spread out over a larger unit and do not have as much time to help each other with reading as they are isolated in separate rooms. It's crucial to emphasize the importance of parental presence in the SFR. Encouraging staff participation in vocal exposure would further enhance this effect.
Demographics and Results between groups
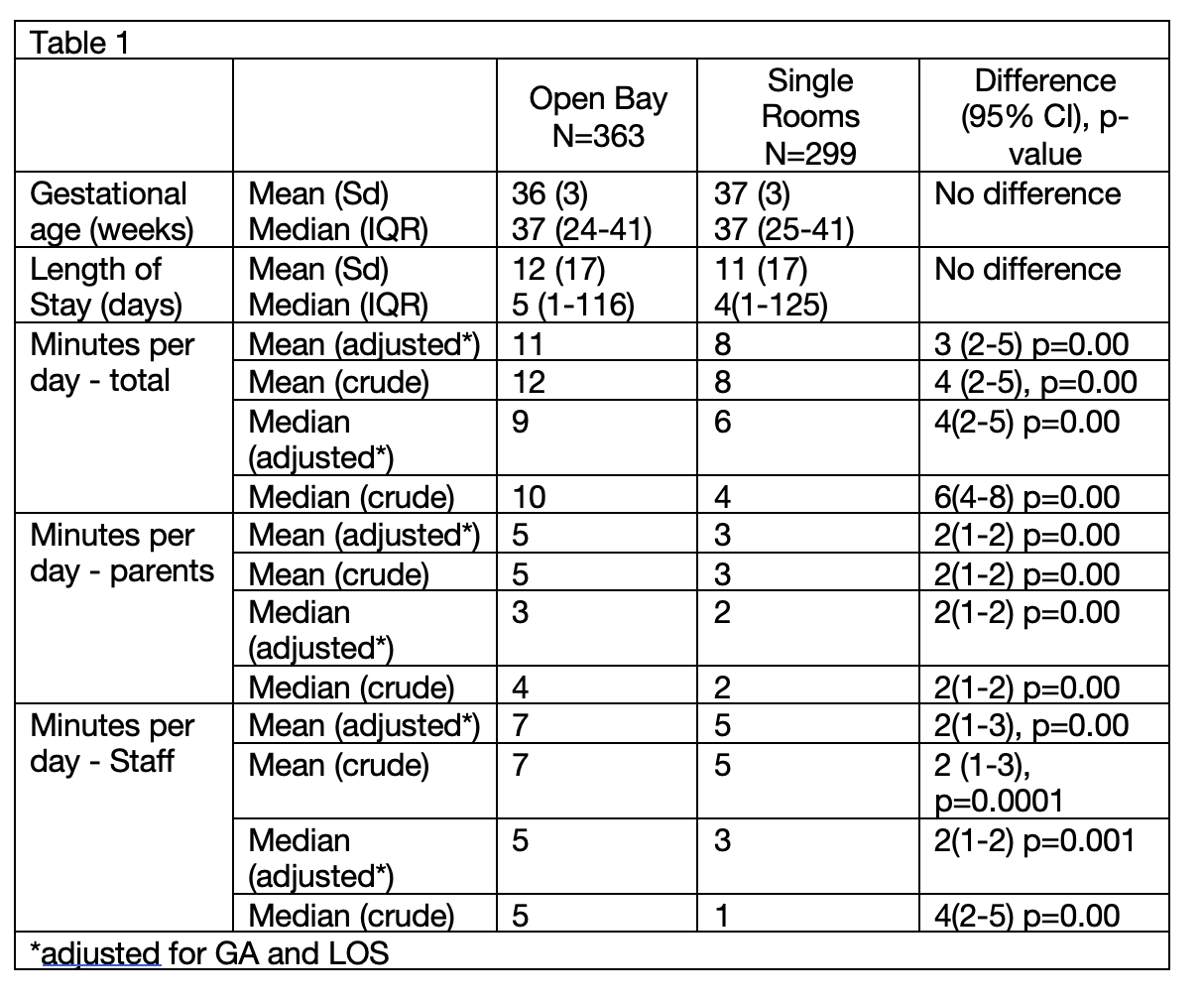 Table 1
Table 1Average Reading Time per day Between Groups
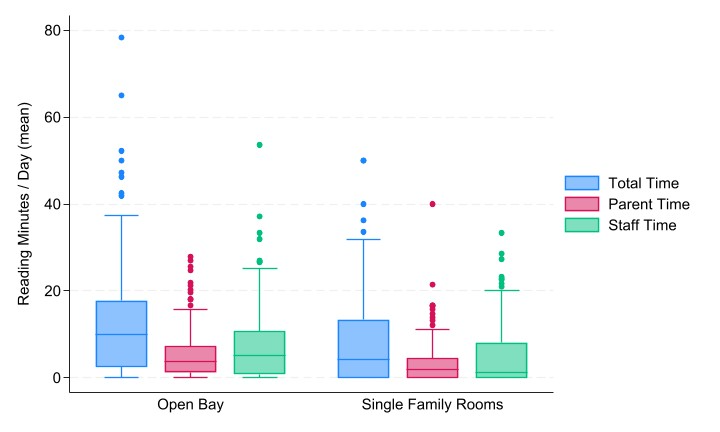 Figure 2
Figure 2Electronic Health Record Flowsheet Documentation
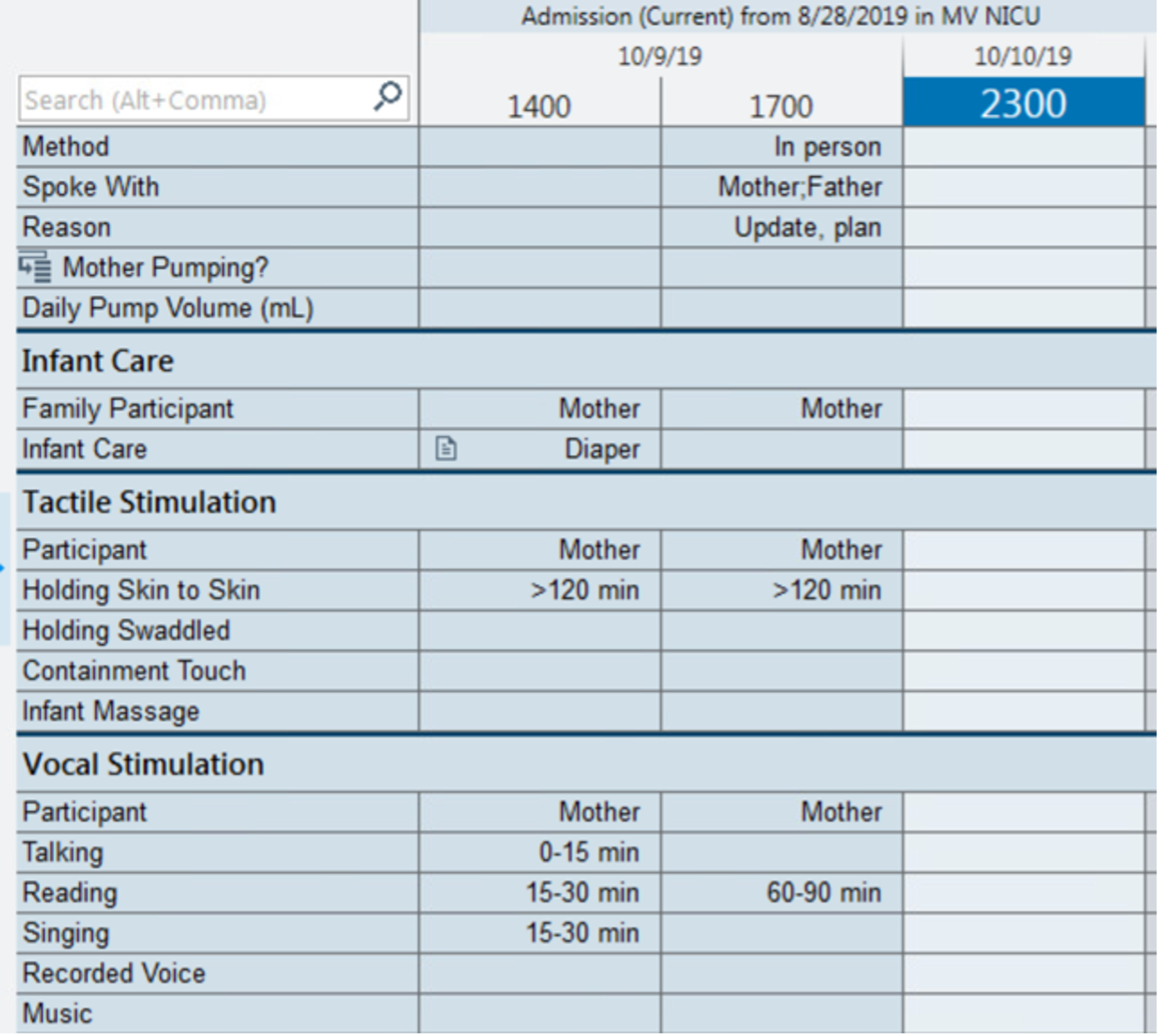 Figure 1
Figure 1
