Neonatal/Infant Resuscitation 1
Session: Neonatal/Infant Resuscitation 1
282 - Use of oxygen for delivery room resuscitation among very preterm infants in China:a multicenter retrospective analysis
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 282.6655
Rujuan Chen, General Hospital of Ningxia Medical University, Yinchuan, Ningxia, China (People's Republic); Jie Yang, Fudan Children's Hospital, China, Shanghai, China (People's Republic); Jianguo Zhou, Children”s Hospital of Fudan university, shanghai, Shanghai, China (People's Republic); Yinping Qiu, General hospital of Ningxia Medical University, Yinchuan, Ningxia, China (People's Republic)
- RC
Rujuan Chen, Ph.D
None
General Hospital of Ningxia Medical University
Yinchuan, Ningxia, China (People's Republic)
Presenting Author(s)
Background: Most guidelines recommended that preterm infants should be given 21% to 40% or 21% to 30% initial oxygen during delivery room resuscitation (DRR) at birth. However, there is few study to survey the actual fraction of inspired oxygen (FiO2) used in very preterm infants (VPIs) in DRR.
Objective: To describe the current status of initial FiO2 used in VPIs in DRR, and the outcomes of different initial FiO2 groups.
Design/Methods: This was a multicenter retrospective analysis. Inborn infants with a gestational age (GA) of < 32 weeks and admitted to 79 tertiary NICUs from the Chinese Neonatal Network (CHNN) within 24h of life between January 1st, 2019 and December 31st, 2021 were enrolled. Infants with major congenital anomalies, unknown oxygen concentration for DRR and palliative care or no active resuscitation due to life-limiting diagnoses were excluded. Infants were divided into four groups according to the initial FiO2 of DRR they received: 1) FiO2 21-30%; 2) FiO2 31-40%;3) FiO2 41-70%; 4) FiO2 71-100%. The maternal and infant characteristics, the distribution of oxygen concentration in different GA and the outcomes among the four FiO2 groups were described. Data were presented as frequencies and percentages or as means/ median with standard deviations (SD)/ interquartile range (IQR), as appropriate. Comparisons between groups were assessed using χ² test for categorical variables and the One-way ANOVA/ Kruskal-Wallis H test for continuous variables.
Results: Of 12347 infants included in this study, 7873 infants (63.8%) received 21-30% initial O2, 2110 infants (17.1%) received 31-40% initial O2, 318 infants (2.6%) received 41-70% initial O2, 2046 infants (16.6%) received 71-100% initial O2. The baseline maternal and infants characteristics in each group were summarized in Table 1. The initial FiO2 varied from 21% to 100% in VPIs, the median value was 40% in GA 24 and GA 25, 30% in other GA groups. With the increase of GA, the IQR showed a decreasing trend, from (30%, 100%) at 24 weeks’ gestation to (21%, 40%) at 31 weeks’ gestation. The proportion of preterm infants used with >30% and >40% FiO2 decreased with increasing GA (Table 2). As the increasing of FiO2, the outcome rates including Apgar score < 7 at 5 min and 10 min, intubation at birth, using epinephrine at birth, maximum oxygen concentration >60% during resuscitation, TRIPS score, invasive ventilation at admission, overall death, ROP≥stage 3, PDA and BPD rates increased (Table 3).
Conclusion(s): VPIs with smaller GA are more likely to receive higher initial FiO2 during DRR. Higher initial FiO2 is associated with some adverse neonatal outcomes.
Table 1 Maternal and infant characteristics among very preterm infants
.jpg) PROM: premature rupture of membranes, ANS: antenatal steroids, IQR: interquartile range, SD: standard deviation, IUGR: intrauterine growth retardation
PROM: premature rupture of membranes, ANS: antenatal steroids, IQR: interquartile range, SD: standard deviation, IUGR: intrauterine growth retardationTable 2 Oxygen concentration of delivery room resuscitation in infants with gestational age <32 weeks in CHNN
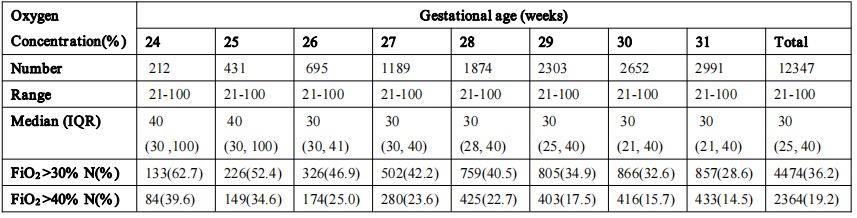
Table 3 Observed rates of neonatal outcomes of very preterm infants across different initial oxygen concentration group
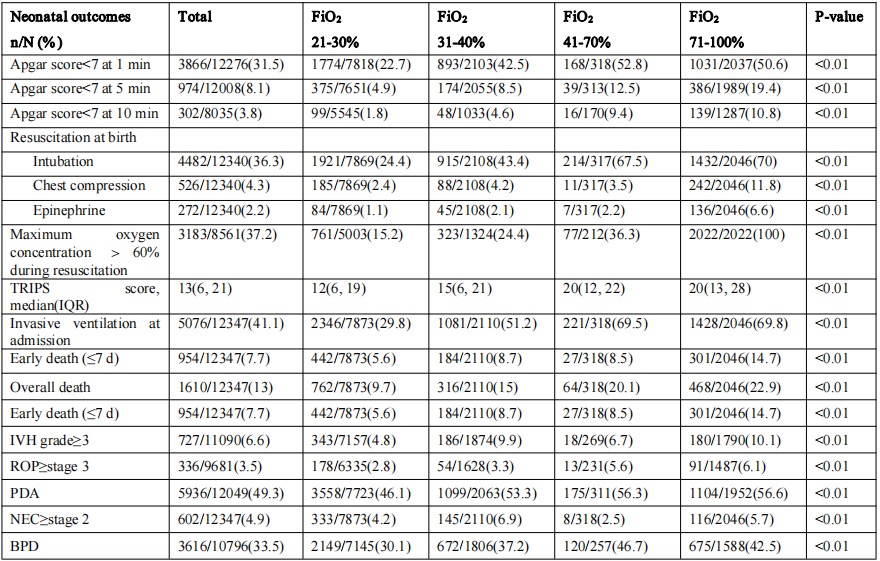 IVH:intraventricular hemorrhage; ROP:retinopathy of prematurity; PDA:patent ductus arteriosus; NEC: Necrotizing enterocolitis; BPD:bronchopulmonary dysplasia
IVH:intraventricular hemorrhage; ROP:retinopathy of prematurity; PDA:patent ductus arteriosus; NEC: Necrotizing enterocolitis; BPD:bronchopulmonary dysplasia
