Neonatal Neurology 3
Session: Neonatal Neurology 3
364 - MRI Findings among Newborns 33 to 35 weeks Gestation following Hypoxic-Ischemic Encephalopathy
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 364.5703
Courtney J. Wusthoff, University of California, Davis, School of Medicine, Sacramento, CA, United States; Carolina V.. Guimaraes, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC, United States; beth Kline-Fath, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Roger G.. Faix, University of Utah School of Medicine, Midvale, UT, United States; Scott A.. McDonald, RTI International, Raleigh, NC, United States; Seetha Shankaran, The University of Texas at Austin, Ann Arbor, MI, United States; Shannon Hamrick, Emory University School of Medicine, Atlanta, GA, United States; Pablo J. Sanchez, Nationwide Children's Hospital -OSU, Columbus, OH, United States; Abhik Das, RTI International, North Potomac, MD, United States; Rosemary Higgins, Florida Gulf Coast University, Fort Myers, FL, United States; Matthew M. Laughon, The University of North Carolina at Chapel Hill, Chapel Hill, NC, United States; Kevin Dysart, Nemours Children's Hospital, PHILADELPHIA, PA, United States; Roy Heyne, University of Texas Southwestern Medical School, Southlake, TX, United States; Stephanie L. Merhar, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Sonia L. Bonifacio, Stanford University School of Medicine, Los Altos, CA, United States; Abbot Laptook, Women & Infants Hospital of Rhode Island, Providence, RI, United States; NICHD Neonatal Research Network, National Institute of Child Health and Human Development, Bethesda, MD, United States

Courtney J. Wusthoff, MD, MS (she/her/hers)
Professor, Neurology
University of California, Davis, School of Medicine
Sacramento, California, United States
Presenting Author(s)
Background: The NICHD Neonatal Research Network trial of therapeutic hypothermia (TH) for HIE in preterm newborns provided prospective, systematic collection and analysis of brain MRI and neurodevelopmental outcomes to address knowledge gaps.
Objective: Assess 1) frequency and severity of brain MRI abnormalities, and 2) relationship between neonatal MRI and neurodevelopment.
Design/Methods: This was a prospective, observational secondary of a randomized trial (TH vs control) for moderate/severe HIE in newborns born 330-356 weeks (wk) gestational age (GA). Included newborns had MRI at 7-21 days postnatal age or died before MRI. Two pediatric neuroradiologists masked to clinical course interpreted images independently; joint review resolved discrepancies. Primary outcome was death or moderate/severe disability at 18-22 months corrected age, defined as Bayley III cognitive score < 85, GMFCS 2-5, seizure disorder, blindness, or hearing loss. Frequency and severity of MRI abnormalities were compared between TH and control; multivariable regressions derived relative risks (RR) and 95% confidence intervals (CI) for select regions. Associations between clinical variables (public insurance, GA, HIE severity, seizures, TH treatment) ± MRI abnormalities and outcome were assessed by multivariable logistic regression; results were adjusted RR (aRR), 95% CI and area under the curve (AUC).
Results: 133 (79%) of 168 newborns were included: 114 had MRI, and 19 died before MRI (TH 11, control 8). TH (n=73, 17 deaths) and control (n=60, 8 deaths) were similar in GA (34.0 ±0.9 vs 34.1 ±0.7 wks), birth weight (2.49 ± 0.68 vs 2.39 ± 0.64 kg), and postmenstrual age at MRI (35.8 ±0.93 vs 35.9 ±0.7 wk). Frequency of abnormal regions among TH infants were highest for white matter (WM), then cerebellum (Cb) and then germinal matrix bleed (GMH). In controls, it was WM, then GMH and then basal ganglia/thalamus (BGT) (Table 1). Cb hemorrhage was more common in TH vs control (p=0.03). Death or Cb hemorrhage was increased 77% in TH (aRR 1.77, 95% CI 1.36-2.29). Severity of abnormalities did not differ between groups (Table 2). AUC for association between clinical variables and death/disability at 18-22 months was 0.8 (Table 3). AUC increased with the addition of WM (0.82) and with BGT instead of WM (0.9).
Conclusion(s): White matter injury predominated among preterm newborns with HIE. TH had a higher risk of Cb hemorrhage vs controls and supports that TH in preterm newborns has important risks. An abnormal BGT improves the prediction of outcome beyond clinical variables alone.
Table 1: Presence of MRI Brain Abnormalities of Any Severity among Infants In the Control and Hypothermia Groups
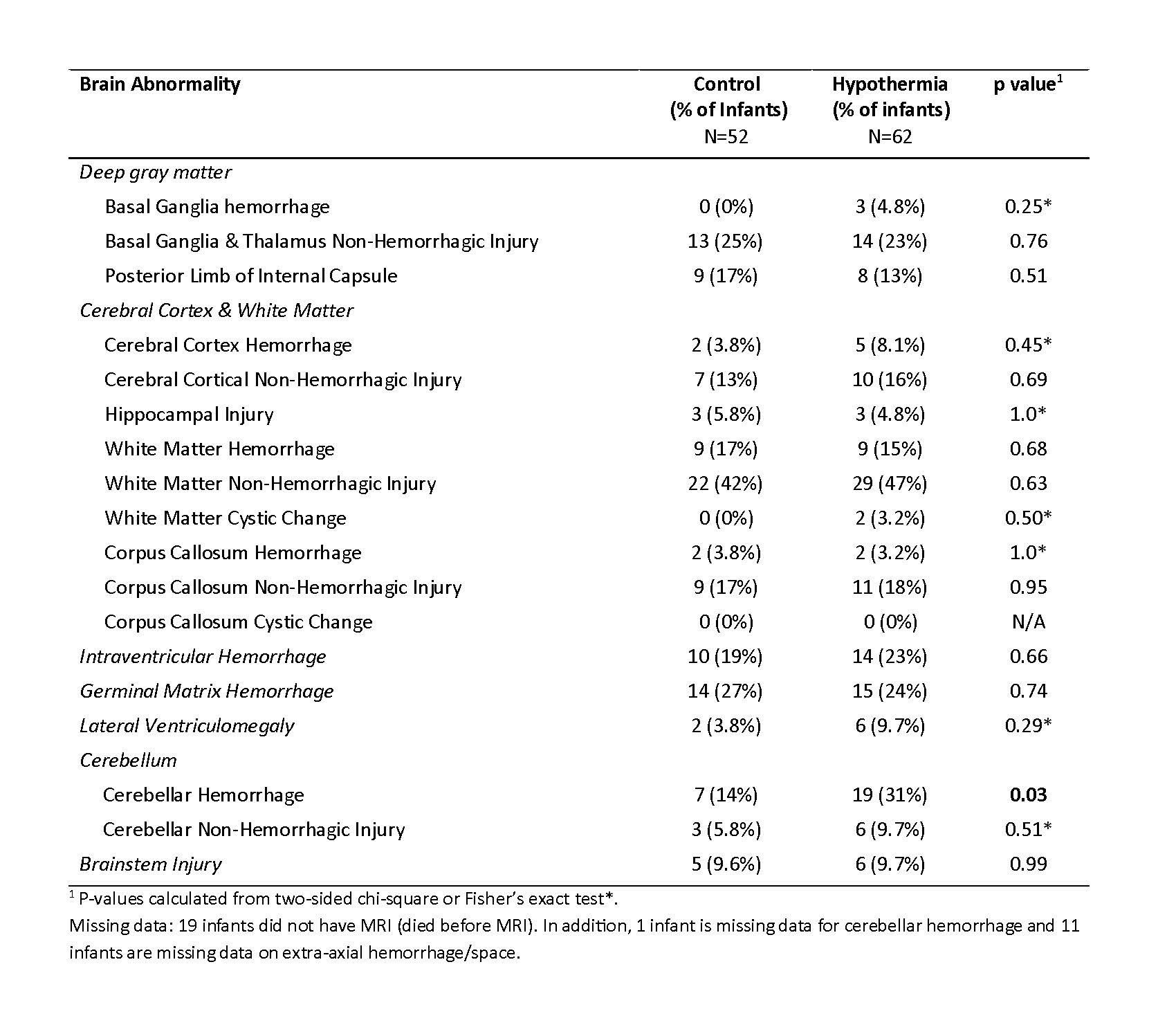
Table 2: Moderate/Severe Brain Abnormalities among Infants in the Control and Hypothermia groups
.jpg)
Table 3: Adjusted Relative Risk of Death or Moderate/Severe Disability at 18-22 months Corrected Age among Infants 33+0 to 35+6 weeks Gestation with and without MRI data
.jpg)

