Neonatal Neurology 1
Session: Neonatal Neurology 1
334 - Effect of Initial Neurosurgical Intervention Timing on Adverse In-hospital Neurologic Outcomes and Death in Preterm Infants with Post-Hemorrhagic Ventricular Dilatation (PHVD)
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 334.4739
Kristen Coletti, Childrens Hospital of Philadelphia, Wynnewood, PA, United States; John Flibotte, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Seetha Shankaran, The University of Texas at Austin, Ann Arbor, MI, United States; Tracy Flanders, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Elizabeth K. Sewell, Emory University School of Medicine; Children's Healthcare of Atlanta, Atlanta, GA, United States; shampa saha, RTI international, Durham, NC, United States; Maria L.V.. Dizon, Lurie Childrens Hospital, Box 45, IL, United States; Mary Catherine E. Gambacorta, Children’s Hospital of Philadelphia, Glen Mills, PA, United States; Andrea F. Duncan, CHOP/Upenn, Philadelphia PA, PA, United States; Sara B.. DeMauro, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; NICHD Neonatal Research Network, National Institute of Child Health and Human Development, Bethesda, MD, United States

Kristen Coletti, MD (she/her/hers)
Neonatologist
Childrens Hospital of Philadelphia
Wynnewood, Pennsylvania, United States
Presenting Author(s)
Background: PHVD is associated with neurodevelopmental impairment (NDI) and death among preterm infants. Recent evidence suggests that early neurosurgical intervention for PHVD leads to improved outcomes.
Objective: To assess whether rates, timing, and type of surgical interventions have changed over time, and identify whether younger postnatal age at first surgery associates with improved in-hospital neurologic outcomes or death in infants with PHVD.
Design/Methods: Retrospective cohort study of infants < 29 weeks GA with PHVD born 1/1/2016-3/31/2024 in the NICHD Neonatal Research Network. We defined surgery as early or late based on median postnatal day at first intervention. The composite primary outcome was death or adverse in-hospital neurologic outcome, defined as meningitis, seizure, or shunt externalization/revision. Data were analyzed using logistic regression and Cochran-Armitage/Jonckheere-Tepstra tests for trends over time.
Results: Of 15,536 infants, 1999 had PHVD, of whom 279 (14%) had neurosurgical intervention. Eighty-one (29%) had only a temporizing device (TD), 90 (32%) had a primary permanent shunt (PS), and 108 (39%) had TD followed by PS (TD-PS), representing 57% conversion from TD to PS. Median postnatal day at first surgery was 33 (IQR 25, 48). The early surgery group ( < 33 days at intervention) had first intervention at 26 days (IQR 22, 28) and the late surgery group at 49 days (IQR 38, 74). Age at first surgery and rate of surgery for PHVD have not changed over time, including when stratified by type of first surgery (Figure 1).
Death or adverse in-hospital neurologic outcome occurred more in the early than late intervention group [31% vs 19%; aOR 1.97 (95% CI 1.09-3.56)] (Table 1). Infants in the late group had more primary PS surgery (43% vs 22%, p=0.0002) and less TD to PS conversion (28% vs 49%, p=0.0005) compared to the early group. Infants with surgical complications of meningitis or shunt externalization/revision were younger at initial surgery (27 vs 34 days, p=0.002) and more likely to have PS as first surgery (47% vs 30%, p=0.04) compared to those without complications. There was no difference in the primary outcome based on initial surgery (TD vs PS) (Table 2). Infants with TD-PS compared to TD alone has a lower rate of the primary outcome [18% vs 28%; aOR 2.06 (95% CI 1.01-4.22)].
Conclusion(s): Rates and timing of neurosurgical intervention for PHVD have not changed over time in the NRN. Surgery at an earlier postnatal age was associated with higher rates of adverse in-hospital neurologic outcomes and death. Future work will explore the relationship between surgical timing and NDI.
Figure 1
.png) Rates, timing and type of neurosurgical interventions for PHVD over time. (A) Postnatal age at first surgical intervention overall and stratified by primary surgery type (TD or PS); (B) Post-menstrual age at first surgical intervention overall and stratified by primary surgery type (TD or PS); (C) Rate of surgical intervention for PHVD over time overall and stratified by primary surgery type (TD or PS); (D) Rate of conversion from TD to PS over time among infants with primary TD. TD, temporizing device; PS, permanent shunt.
Rates, timing and type of neurosurgical interventions for PHVD over time. (A) Postnatal age at first surgical intervention overall and stratified by primary surgery type (TD or PS); (B) Post-menstrual age at first surgical intervention overall and stratified by primary surgery type (TD or PS); (C) Rate of surgical intervention for PHVD over time overall and stratified by primary surgery type (TD or PS); (D) Rate of conversion from TD to PS over time among infants with primary TD. TD, temporizing device; PS, permanent shunt.Table 1: Adverse In-hospital Outcomes for Infants with Early versus Late Surgical Intervention
.png) * Adjusted Odds ratio (95% CI) for categorical outcomes were obtained using Logistic regression. Parameter estimates (95% CI) for continuous outcomes were obtained using generalized linear model. All models were adjusted for gestational age, gender, race and antenatal steroids. The odds ratio and parameter estimates compare Early Intervention vs. Late Intervention.
* Adjusted Odds ratio (95% CI) for categorical outcomes were obtained using Logistic regression. Parameter estimates (95% CI) for continuous outcomes were obtained using generalized linear model. All models were adjusted for gestational age, gender, race and antenatal steroids. The odds ratio and parameter estimates compare Early Intervention vs. Late Intervention.Table 2: Adverse In-hospital Outcomes for Infants with Primary TD versus Primary PS
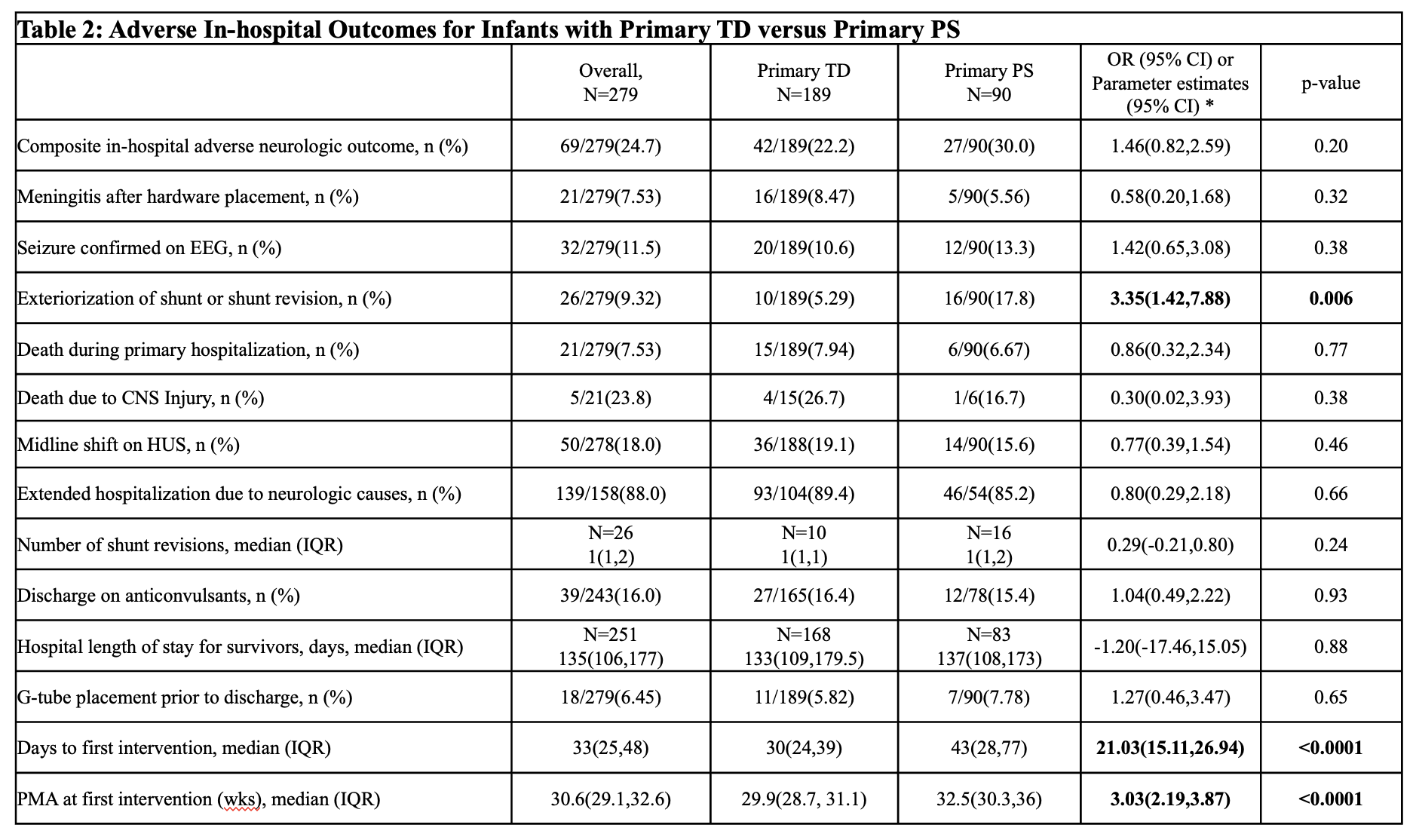 * Adjusted Odds ratio (95% CI) for categorical outcomes were obtained using Logistic regression. Parameter estimates (95% CI) for continuous outcomes were obtained using generalized linear model. All models were adjusted for gestational age, birth weight, gender, and race. The odds ratio and parameter estimates compare Primary PS vs. Primary TD.
* Adjusted Odds ratio (95% CI) for categorical outcomes were obtained using Logistic regression. Parameter estimates (95% CI) for continuous outcomes were obtained using generalized linear model. All models were adjusted for gestational age, birth weight, gender, and race. The odds ratio and parameter estimates compare Primary PS vs. Primary TD.
