Neonatal/Infant Resuscitation 2
Session: Neonatal/Infant Resuscitation 2
300 - Comparison of a Rapid Volume Infusion Versus Standard Care During Advanced Cardiopulmonary Resuscitation of Moderately Asphyxiated Lambs.
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 300.4346
Graeme Polglase, Monash University, Melbourne, Victoria, Australia; Nhi Tran, The Ritche Centre, The Hudson Institute of Medical Research, Melbourne, Victoria, Australia; Stuart B. Hooper, Monash University, Black Rock, Victoria, Australia; Martin Kluckow, Sydney University, Sydney, New South Wales, Australia; Andrew W. Gill, University of Western Australia, Subiaco, Western Australia, Australia; Georg Schmölzer, University of Alberta Faculty of Medicine and Dentistry, Edmonton, AB, Canada; Calum T. Roberts, Monash University, Clayton, Victoria, Australia
- GP
Graeme Polglase, PhD (he/him/his)
Professor, Deputy Centre Head
Monash University
Melbourne, Victoria, Australia
Presenting Author(s)
Background: Birth asphyxia remains a major cause of neonatal mortality. The key to successful return of spontaneous circulation (ROSC) is increased coronary blood flow from raised end-diastolic blood pressure.
Objective: To determine whether a rapid infusion of saline during advanced CPR, compared to standard intravenous (IV) Epinephrine, increases diastolic blood pressure, achieves return of spontaneous circulation (ROSC), maintains physiological stability after ROSC and reduces cerebral micro-haemorrhages.
Design/Methods: Near-term newborn lambs (0.93 gestation) were asphyxiated until mean blood pressure reached 10-12 mmHg and heart rate was < 60 bpm. Resuscitation was commenced with positive pressure ventilation (VG 7 ml/kg) and chest compressions commenced 1 min later. Lambs were randomised to: Standard Care (20 micrograms/kg IV Epinephrine; n=8) or Volume Infusion (saline; 20 ml/kg given over 30s; n=10) starting 1 min after chest compressions. After 2 allocated volume infusions 3 min apart, rescue IV Epinephrine was administered if ROSC was not achieved by 8 min. Lambs achieving ROSC were monitored for 60 min. Cerebral histology was assessed for micro-haemorrhages within white and grey matter regions.
Results: ROSC occurred in 8/8 Standard Care and 8/10 Volume Infusion lambs, although 3 required rescue Epinephrine to achieve ROSC. Mean and diastolic blood pressure (Fig 1A, B) and cerebral blood flow were higher in Volume Infusion lambs during CPR. After ROSC, blood pressure (Fig 1C), heart rate and arterial PaO2 were transiently higher in Standard Care compared to Volume Infusion lambs. At autopsy, Volume Infusion lambs had higher brain weights (by 6.7%) and increased number of micro-haemorrhages within the periventricular white matter (p=0.027), but not in other regions.
Conclusion(s): Volume Infusion was inferior to standard care in achieving ROSC and reducing cerebral micro-haemorrhages. The use of volume infusion alone during CPR in moderately asphyxiated newborns is likely not appropriate for clinical implementation.
Figure 1
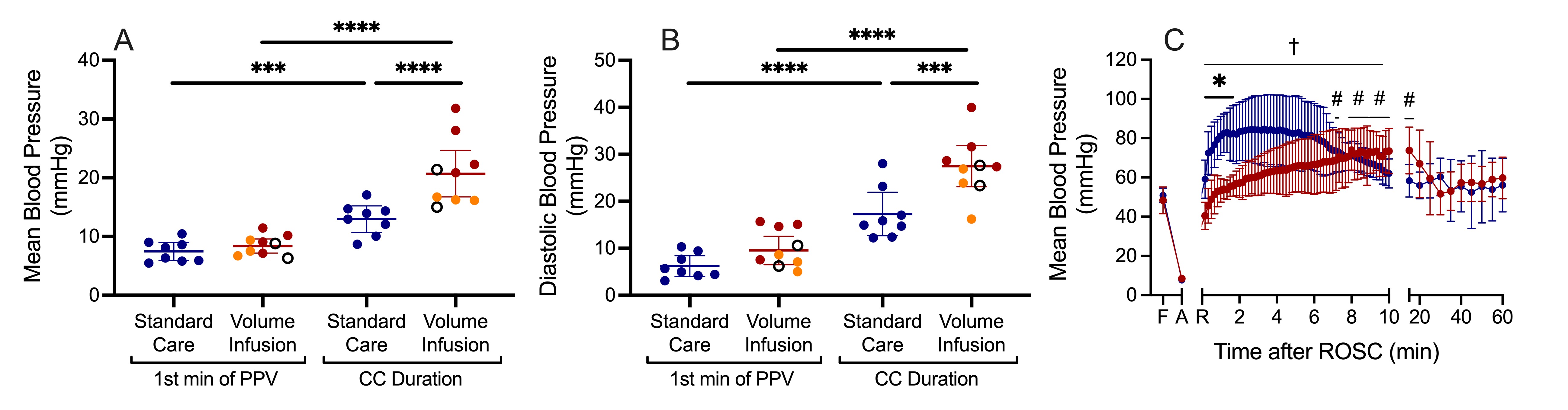 Figure 1: A) Mean and B) Diastolic blood pressure during the first minute of positive pressure ventilation and throughout chest compressions in Standard Care (blue) and Volume Infusion (red) lambs. Note, Volume Infusion lambs in orange required rescue Epinephrine and open circles represent lambs that did not achieve ROSC. C) Mean blood pressure after ROSC – note the overshoot of blood pressure in Standard Care lambs.
Figure 1: A) Mean and B) Diastolic blood pressure during the first minute of positive pressure ventilation and throughout chest compressions in Standard Care (blue) and Volume Infusion (red) lambs. Note, Volume Infusion lambs in orange required rescue Epinephrine and open circles represent lambs that did not achieve ROSC. C) Mean blood pressure after ROSC – note the overshoot of blood pressure in Standard Care lambs.
