Neonatal Neurology 2
Session: Neonatal Neurology 2
348 - Family Social Risks on Neurodevelopmental Outcomes in Extremely Preterm Infants Without Severe Brain Injury
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 348.4829
Li-Wen Chen, National Cheng Kung Univertisy, College of Medicine, Tainan, Tainan, Taiwan (Republic of China); Min-Lan Tsai, Taipei Medical University Hospital, Taipei, Taipei, Taiwan (Republic of China); Yung-Chieh Lin, National Cheng Kung University Hospital, Tainan, Tainan, Taiwan (Republic of China); Chi-Hsiang Chu, National University of Kaohsiung, Kaohsiung, Kaohsiung, Taiwan (Republic of China); Chao-Ching Huang, National Cheng Kung University Hospital, Taiwan, Tainan City, Tainan, Taiwan (Republic of China)
- LC
Li-Wen Chen, MD PhD (she/her/hers)
Attending Physician
National Cheng Kung Univertisy Hospital
Tainan, Tainan, Taiwan (Republic of China)
Presenting Author(s)
Background: Even without severe neonatal brain injury (SNBI), extremely preterm (EP) infants still face a high rate of neurodevelopmental impairment (NDI) outcome. How family social risks interact with neonatal critical illnesses and conjunctively impact NDI outcomes remains unclear.
Objective: To explore the role of family social environment on neurodevelopmental outcomes in EP infants.
Design/Methods: The population-based cohort study analyzed EP infants without SNBI who were born in 2011 to 2022 and assessed for cognitive, language, and motor development at age 6, 12 and 24 months using the Bayley Scales of Infant Development, third edition. The multicenter population cohort enrolled EP infants in a geographic-defined area of southern Taiwan. Infants born at < 29 weeks’ of gestation but without high-grade intraventricular hemorrhage, cystic periventricular leukomalacia, or bilateral cerebellar hemorrhage were included for analysis. The family-social risk index included maternal age at childbirth < 21 years, maternal education below university, low family socioeconomic status, maternal minority ethnicity, and single-parent. Clinical risks included perinatal complications and neonatal morbidities. NDI was categorized by degrees of cognitive and motor delay, cerebral palsy, and neurosensory deficits at age 24 months. Ordered logistic regression and multivariable models were used to evaluate risk factors for NDI severity.
Results: Among 459 infants, 82% had no/mild NDI, 14% had moderate NDI, and 4% had severe NDI. Principal component analysis of the linear combination of developmental scores at 12 months revealed significant differences between the no/mild NDI and moderate/severe NDI groups. Infants with family social risks had 2.07 times higher odds (95% CI: [1.23, 3.54]) of more severe NDI, and each extra day of oxygen therapy increased NDI risk by 3% (95% CI: [2%, 4%]). Family social risks significantly lowered cognitive (by 6.25), language (by 5.31), and motor (by 3.46) scores. Males had lower cognitive (by 2.65) and language (by 4.07) scores than females. Each additional day of oxygen therapy reduced scores in all three domains by 0.09-0.12, and severe necrotizing enterocolitis decreased motor scores by 2.84.
Conclusion(s): In EP infants without SNBI, family social risks and male had a greater negative impact on neurodevelopmental outcomes than clinical factors. Implementing developmental surveillance could help identify high-risk infants for later NDI.
Figure 1
.jpg) Differences in the developmental trajectory of cognition (A), language (B), and motor (C) performance from corrected age 6 months, 12 months to 24 months among the three neurodevelopmental impairment (NDI) outcome groups of extremely preterm infants without severe neonatal brain injury.
Differences in the developmental trajectory of cognition (A), language (B), and motor (C) performance from corrected age 6 months, 12 months to 24 months among the three neurodevelopmental impairment (NDI) outcome groups of extremely preterm infants without severe neonatal brain injury. Figure 2
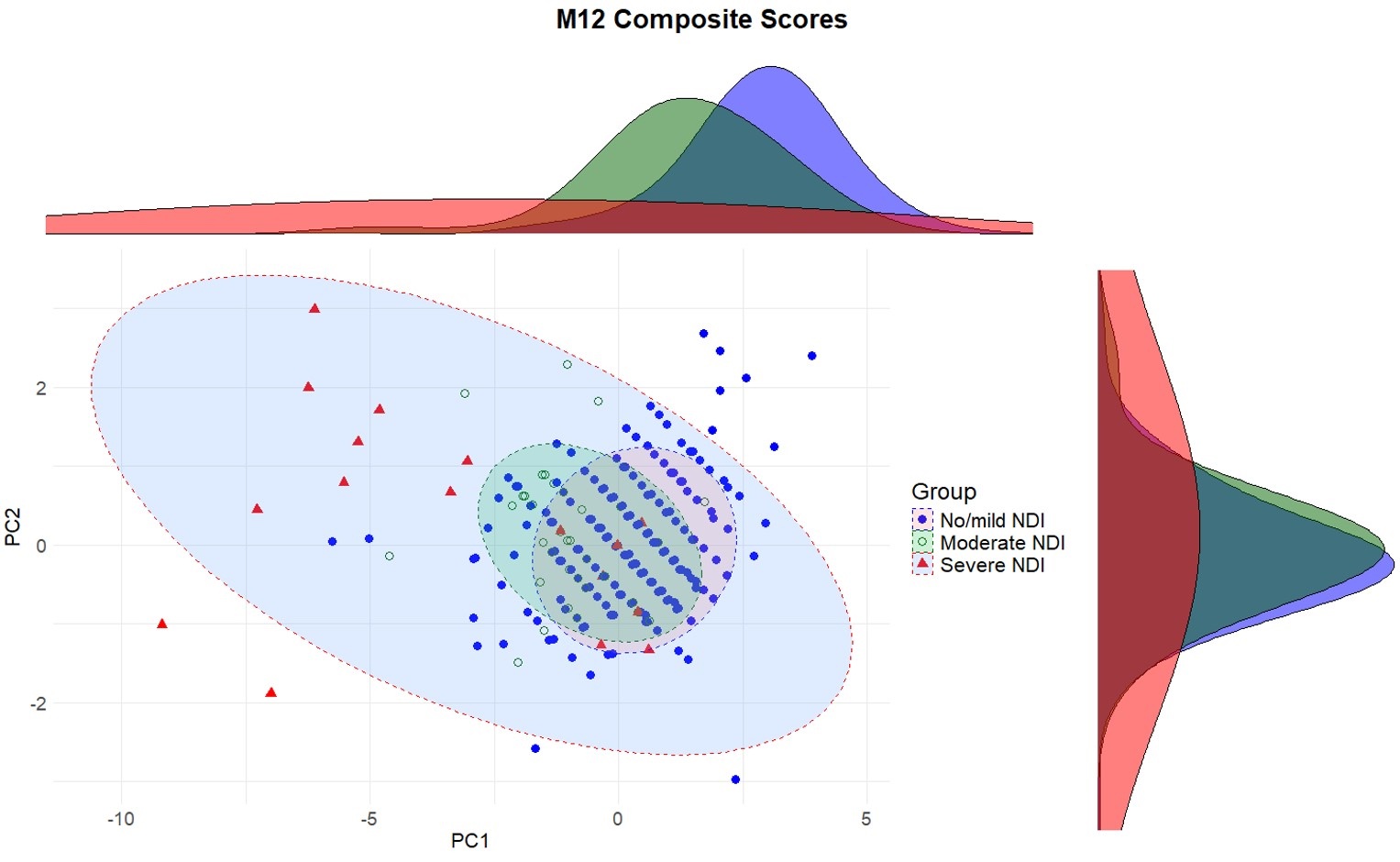 Principal component (PC) analysis using cognitive, language, and motor developmental performances at age 12 months (M12) for NDI outcomes at 24 months of age.
Principal component (PC) analysis using cognitive, language, and motor developmental performances at age 12 months (M12) for NDI outcomes at 24 months of age. Table 1
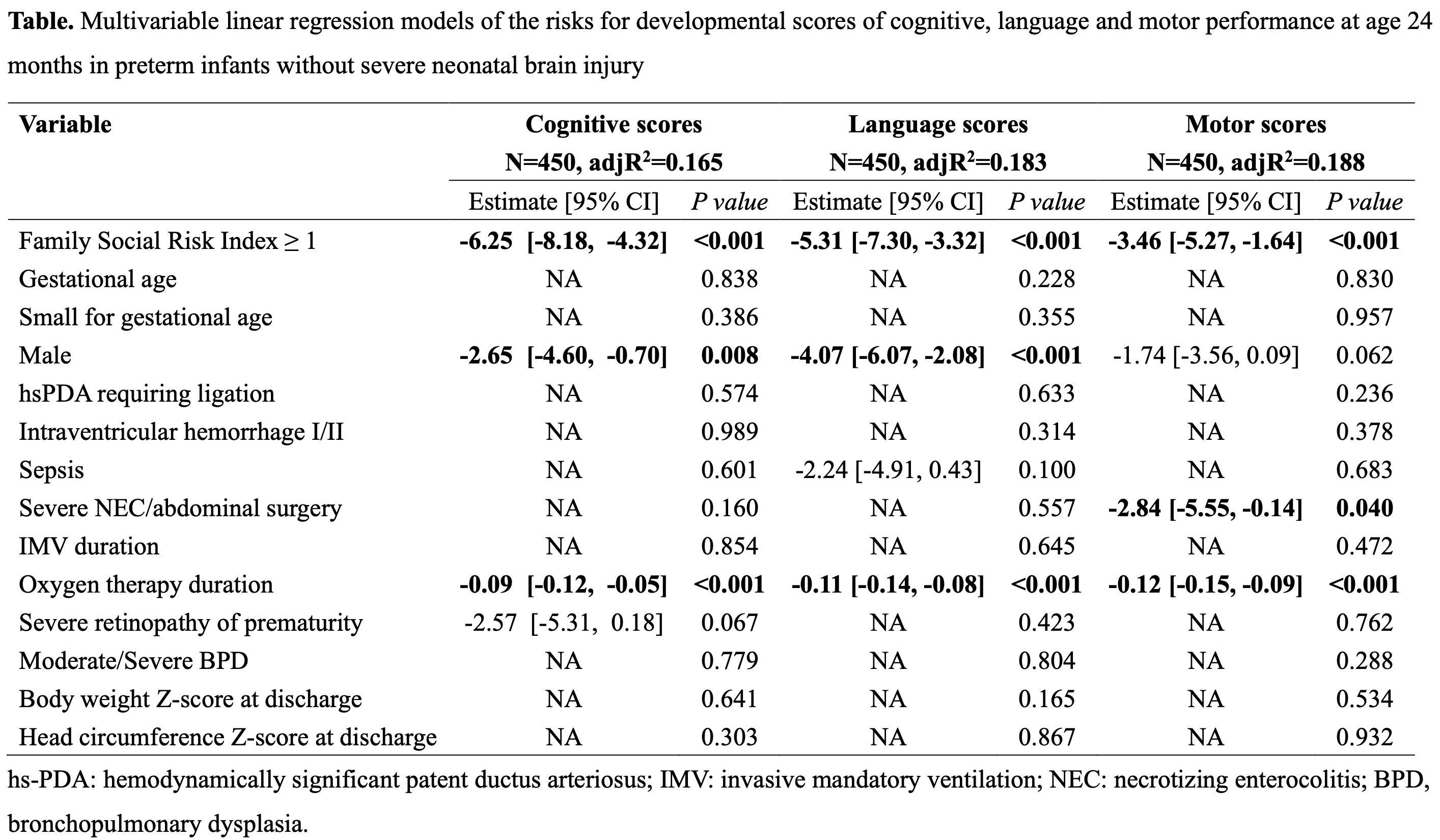 Multivariable linear regression models of the risks for developmental scores of cognitive, language and motor performance at age 24 months in extremely preterm infants without severe neonatal brain injury
Multivariable linear regression models of the risks for developmental scores of cognitive, language and motor performance at age 24 months in extremely preterm infants without severe neonatal brain injury 
