Global Neonatal & Children's Health 1
Session: Global Neonatal & Children's Health 1
725 - Machine Learning Approaches to Identify Neonates at Risk for Post-Discharge Mortality in Dar es Salaam, Tanzania and Monrovia, Liberia
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 725.5660
Chris A. Rees, Emory University School of Medicine, Atlanta, GA, United States; Rodrick R. Kisenge, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Dar es Salaam, Tanzania; Evance Godfrey, Muhimbili National Hospital, Dar es salaam, Dar es Salaam, Tanzania; Readon C. Ideh, JFK Medical Center, Monrovia, Montserrado, Liberia; Ye-Jeung G.. Coleman-Nekar, John F. Kennedy Medical Center, Monrovia, Montserrado, Liberia; Abraham Samma, Muhimbili University of Health and Allied Sciences, Griffith, Australian Capital Territory, Australia; Hussein K. Manji, The Aga Khan Hospital Dar es salaam, Dar es salaam, Dar es Salaam, Tanzania; Christopher Sudfeld, Harvard T. H. Chan School of Public Health, Boston, MA, United States; Adrianna Westbrook, Emory University School of Medicine, Atlanta, GA, United States; Michelle Niescierenko, Boston Children's Hospital, Boston, MA, United States; Claudia R.. Morris, Emory University School of Medicine, Atlanta, GA, United States; Todd A. Florin, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Rishikesan Kamaleswaran, Duke University School of Medicine, Durham, NC, United States; Christopher Duggan, Boston Children's Hospital, Boston, MA, United States; Karim Manji, Muhimbili University of Health and Allied Sciences, Dar-es-Salaam, Dar es Salaam, Tanzania
- CR
Chris A. Rees, MD, MPH
Assistant Professor
Emory University School of Medicine
Atlanta, Georgia, United States
Presenting Author(s)
Background: The time after hospital discharge carries high rates of mortality among neonates in sub-Saharan Africa. Traditional logistic regression models to identify neonates at risk for post-discharge mortality have yielded only fair discriminatory value.
Objective: To determine if machine learning models yield greater discriminatory value than a traditional logistic regression model to identify neonates at risk for post-discharge mortality
Design/Methods: We conducted a prospective observational cohort study including neonates (aged 0-28 days) discharged from Muhimbili National Hospital in Dar es Salaam, Tanzania and John F. Kennedy Medical Center in Monrovia, Liberia (2019-2022). We collected data on candidate variables during hospital admission and followed neonates to ascertain all-cause, 60-day post-discharge mortality. We used machine learning approaches (i.e., extreme gradient boost, hist gradient boost, support vector machine, and neural networks) to develop risk assessment models to identify neonates at risk for post-discharge mortality. We plotted the relative contribution of each variable through Shapley plots, determined the discriminatory value of each model through area under the receiver operating characteristic curves (AUC), and compared the chance of post-discharge mortality in each model to the area under the precision recall curves (AUPRC).
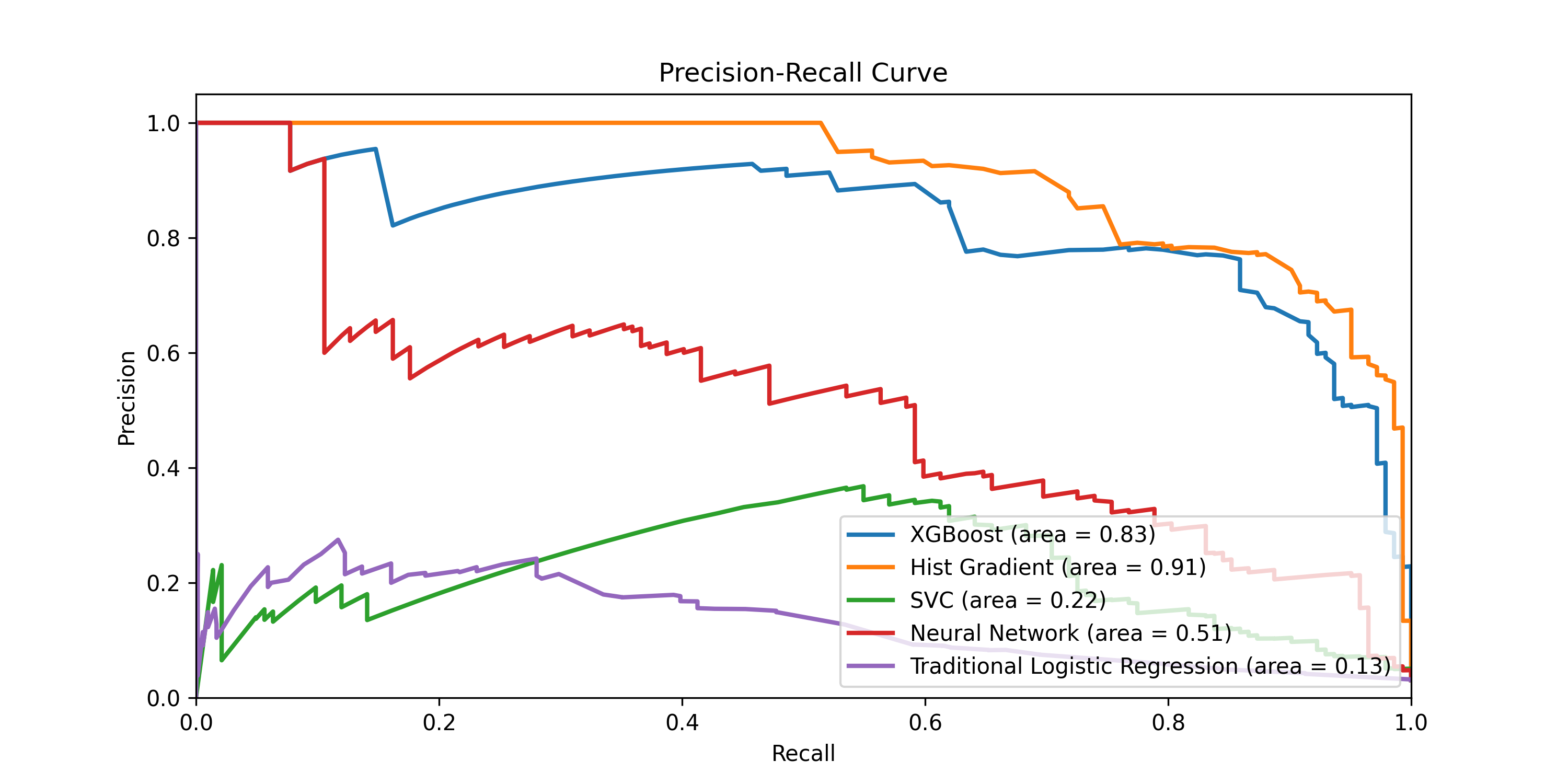
Results: A total of 2,294 neonates enrolled and had 60-day outcomes available. Of these, 71 (3.1%) died within 60 days after hospital discharge. The hist gradient model, which included four clinical features (weight at admission, receipt of supplemental oxygen during hospital admission, discharge against medical advice, and presence of congenital birth defects) and two social features (caregiver age and caregiver highest education; Fig 1), yielded the greatest discriminatory value (AUC 0.995; P< 0.001 compared to logistic regression; Fig 2). Discharge against medical advice, low birth weight, and supplemental oxygen requirement during hospitalization were predictive of post-discharge mortality in all models. All models demonstrated AUPRCs above baseline chance of post-discharge mortality (Fig 3).
Conclusion(s): Our parsimonious machine learning models had excellent discriminatory value to predict all-cause, 60-day post-discharge mortality among neonates in two large hospitals in sub-Saharan Africa. Machine learning models had greater discriminatory value than traditional logistic regression modeling. External validation of these models is warranted to assist in the design of appropriate tools and interventions to reduce mortality in this vulnerable population.
Fig 1. Shapley plots of the relative contribution of each feature to identify neonates at risk for post-discharge mortality
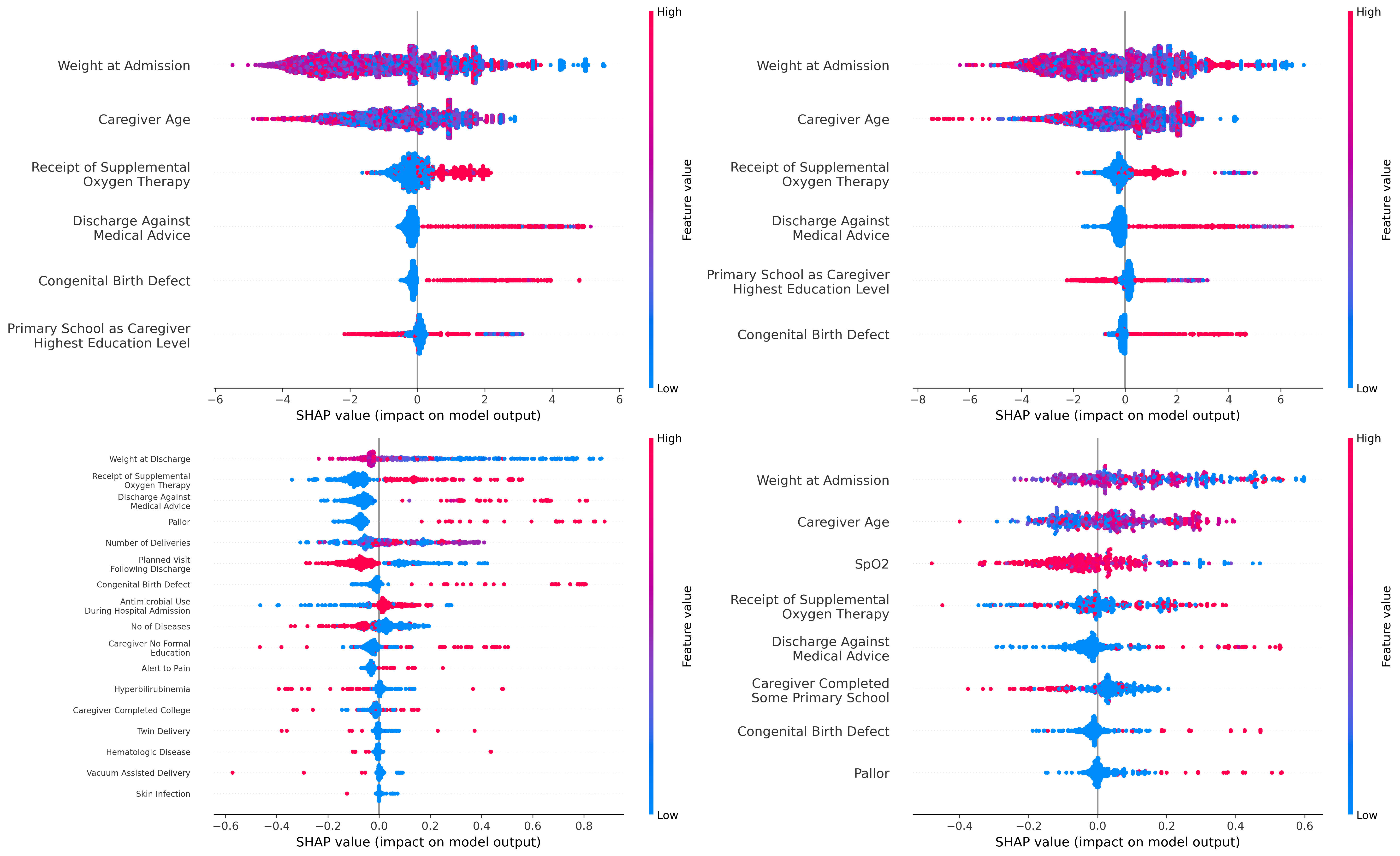
Fig 2. Discriminatory value of machine learning models to identify neonates at risk for post-discharge mortality
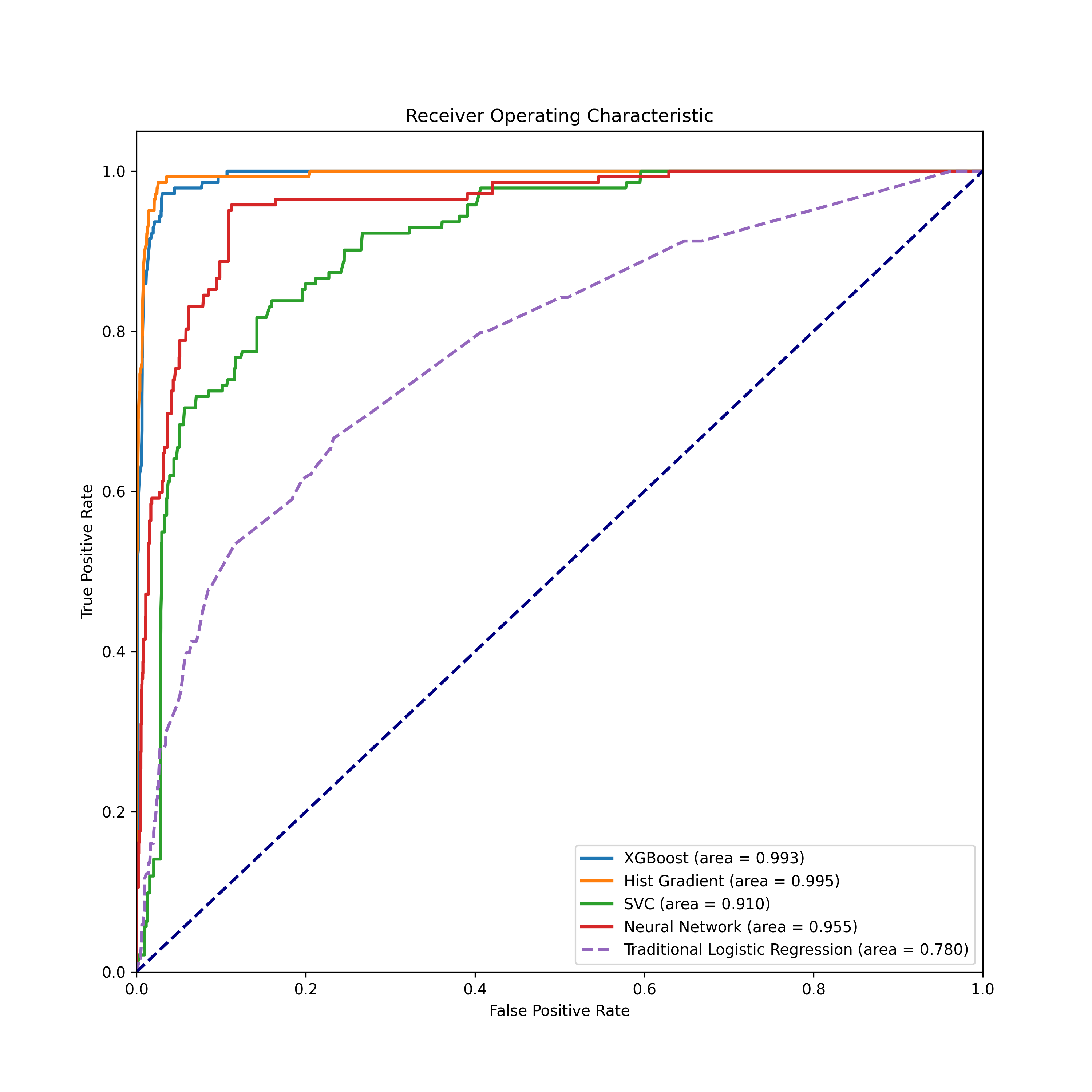
Fig 3. Area under the precision-recall curves for machine learning models to identify neonates at risk for post-discharge mortality