Neonatal/Infant Resuscitation 2
Session: Neonatal/Infant Resuscitation 2
302 - Post-resuscitation hemodynamics following cardiac arrest vs. bradycardia: Role of saline bolus.
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 302.6376
Rebecca Valdez, University of California Davis, Davis, CA, United States; Evan M. Giusto, UC Davis Health, Sacramento, CA, United States; Amy Lesneski, University of California, Davis, School of Medicine, Davis, CA, United States; Victoria Hammitt, University of California, Davis, School of Medicine, Sacramento, CA, United States; Michelle J. Lim, University of California, Sacramento, CA, United States; Jessa Rose A. Li, University of California Davis Children's Hospital, Sacramento, CA, United States; Erika N.. Zerda, University of California, Davis, School of Medicine, Sacramento, CA, United States; Paulina Hume, University of California Davis Children's Hospital, 612 El Dorado Way, CA, United States; Sylvia Bowditch, University of California Davis Children's Hospital, Sacramento, CA, United States; Erin Riley, University of California, Davis, School of Medicine, Redding, CA, United States; Satyan Lakshminrusimha, UC Davis, Sacramento, CA, United States; Deepika Sankaran, University of California Davis Children's Hospital, Sacramento, CA, United States

Rebecca Valdez, B.S. (she/her/hers)
Trainee
University of California Davis
Davis, California, United States
Presenting Author(s)
Background: Extremely preterm infants are at risk of respiratory distress syndrome and circulatory impairments after birth (Sehgal et al 2023). Excess fluid administration is associated with increased risk of intraventricular hemorrhage (IVH) in preterm infants. It is not known if rapid administration of saline boluses after birth induce fluctuation in cerebral blood flow that may potentially increase the risk of developing an IVH.
Objective: To compare the post-resuscitation hemodynamics after asphyxial arrest and bradycardia vs non-asphyxiated controls and assess the effect of saline bolus over 5-min and 2-min on fluctuation in carotid artery blood flow.
Design/Methods: Preterm gestation (127 days) fetal lambs were intubated and instrumented. Fifteen lambs were randomized to (1) non-asphyxiated controls, or by asphyxia induced by umbilical cord occlusion to (2) bradycardia or heart rate < 60 bpm, or (3) asystole or heart rate=0. Lambs were resuscitated per NRP guidelines. After return of spontaneous circulation (ROSC), all lambs were randomized to receive a 10-mL/kg normal saline bolus over 2-minutes or 5-minutes or no bolus in a random sequence at 10, 20 or 30 minutes after birth. Hemodynamics and blood gases were monitored.
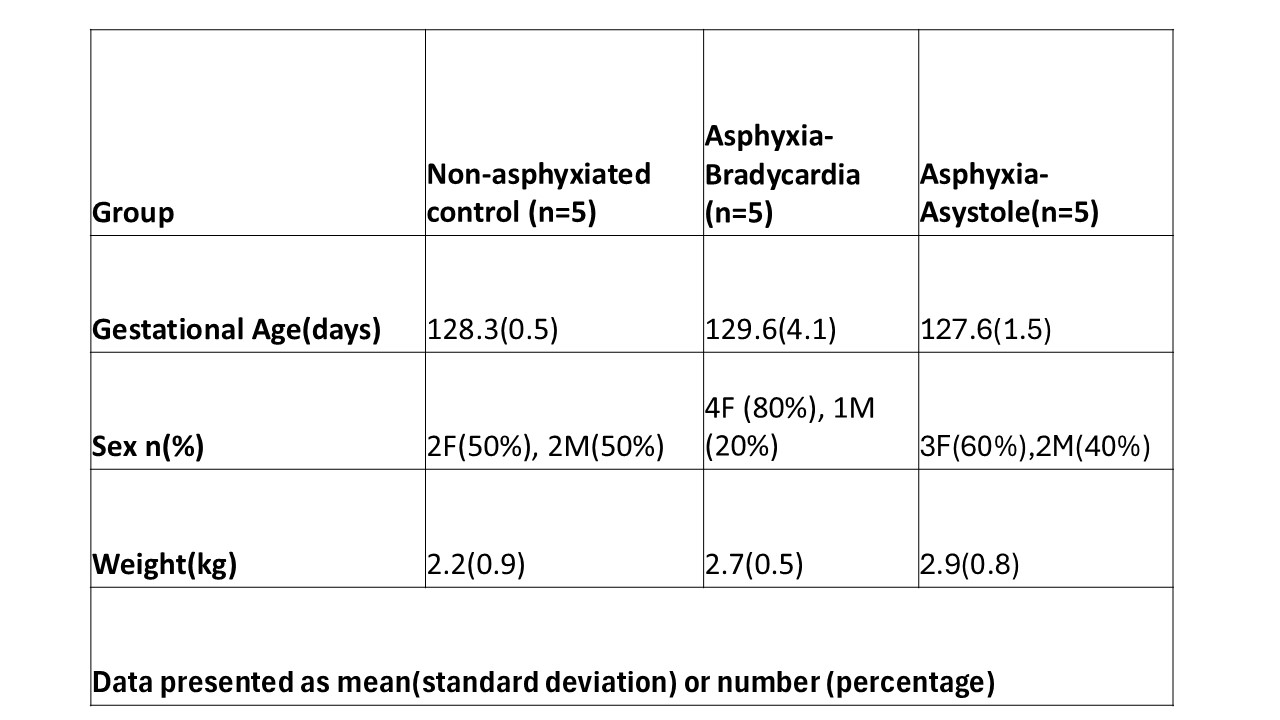
Results: The baseline characteristics including birth weight and sex were not different between the 3 groups (table). All asystolic lambs required 1 dose of intravenous epinephrine to achieve ROSC. The left carotid artery blood flow (CaF) was lower in the asystole and bradycardia groups. Carotid blood flow improved by 5 minutes after ROSC but decreased in the bradycardia group beyond 15 minutes after ROSC (figure 1a). The mean blood pressure and heart rate were not different in non-asphyxiated controls compared to asystole and bradycardia groups during the post-ROSC period (figure 1b and 1c). Percentage fluctuation in CaF was 130 (46), 215 (105) and 155 (29)% of pre-bolus baseline with the 10-mL/kg bolus over 5-min, and 120 (47), 174 (13) and 160 (41)% with the 10-mL/kg bolus over 2-min in non-asphyxiated control, bradycardia, and asystole groups respectively.
Conclusion(s): Saline boluses over 5-min and 2-min are associated with similar fluctuations in blood flow to the brain in non-asphyxiated, as well as asphyxiated lambs with bradycardia and asystole. Further studies are needed to assess the impact of fluctuation in CaF on IVH, survival and neurodevelopmental outcomes.
Comparison of left carotid artery blood flow (1a), mean blood pressure (1b), and heart rate (1c) between three groups of preterm lambs (non-asphyxiated control, asphyxia asystole, asphyxia bradycardia).
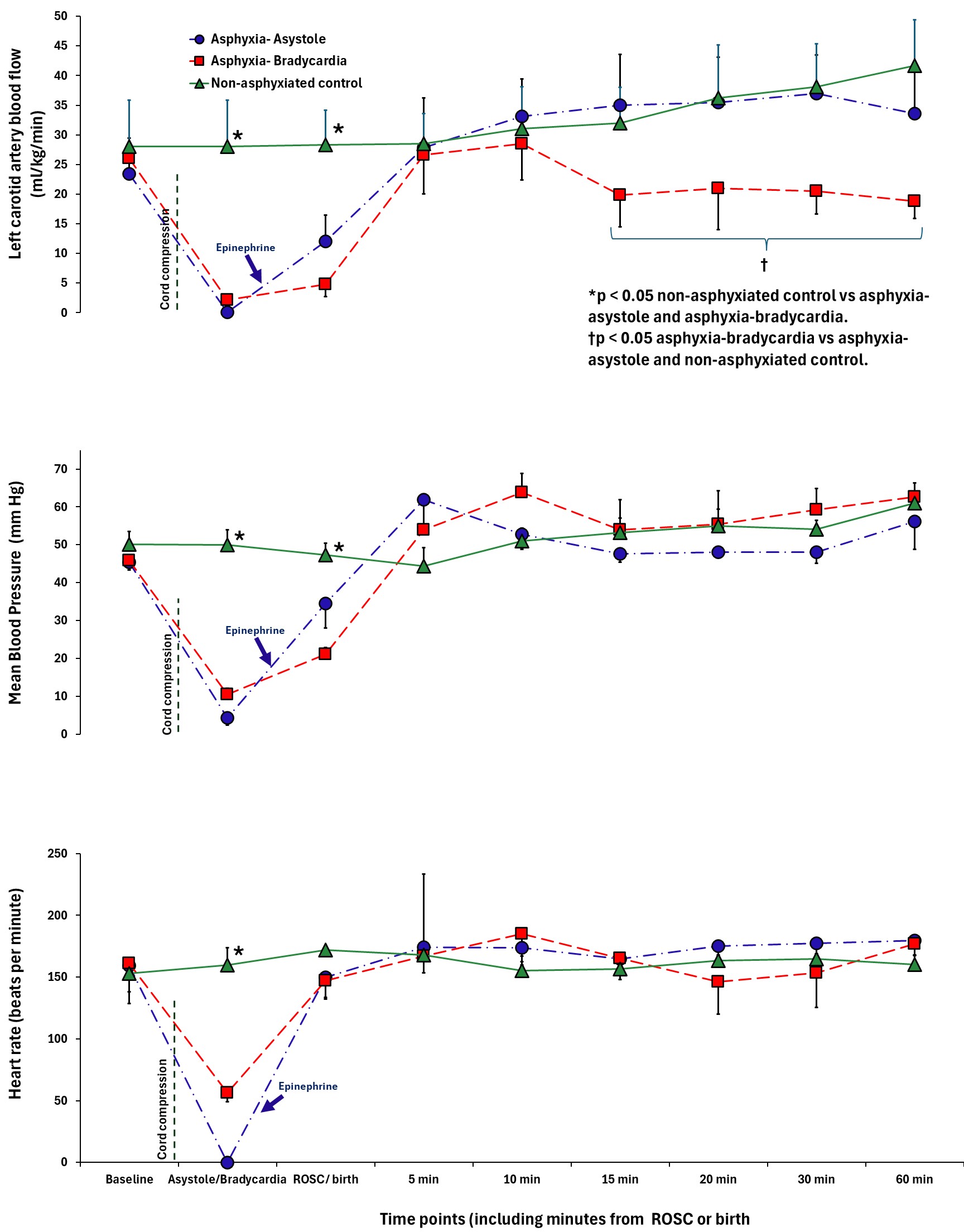 Blue arrow represents the timing of epinephrine following chest compressions for the asystolic lambs. Although mean blood pressure and heart rate were not different after ROSC, the left carotid artery blood flow was significantly lower in the lambs asphyxiated to bradycardia.
Blue arrow represents the timing of epinephrine following chest compressions for the asystolic lambs. Although mean blood pressure and heart rate were not different after ROSC, the left carotid artery blood flow was significantly lower in the lambs asphyxiated to bradycardia. Comparison of baseline characteristics