Neonatal General 1: Respiratory, BPD
Session: Neonatal General 1: Respiratory, BPD
272 - Influence of flow rate change on CO2 levels during high flow nasal ventilation (HFNV) in preterm infants.
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 272.5114
Ori Hochwald, Rambam Medical Center, Haifa, Israel, Haifa, Hefa, Israel; Christopher Farah, Rambam Hospital . Haifa. Israel, Haifa, Hefa, Israel; Liron Borenstein-Levin, Rambam Medical Center, haifa, Hefa, Israel; Yoav Littner, Rambam Medical center, Haifa, Hefa, Israel; Mordechai A. Kugelmann, Rambam Medical Center, Haifa, Haifa, Hefa, Israel
- OH
Ori Hochwald, MD (he/him/his)
Head of NICU
Rambam Medical Center, Haifa, Israel
Haifa, Hefa, Israel
Presenting Author(s)
Background: Heated, humidified, high-flow nasal ventilation (HFNV) is a popular method of non-invasive respiratory support. The HFNV flow rate is defined as exceeding the patient's peak inspiratory flow rate, which provides an accurate FiO2 and facilitates dead space washout. However, the effect of altering the flow rate on CO2 levels remains uncertain and has not been extensively studied.
Objective: To assess changes in CO2 levels, measured by transcutaneous CO2 (tcCO2), in preterm infants receiving HFNV at either a "low" flow rate (2 LPM) or a "high" flow rate (6 LPM).
Design/Methods: Following a 3-hour stabilization period at either a high (6 LPM) or low (2 LPM) flow rate, preterm infants on HFNV were monitored using tcCO2 over consecutive 3-hour periods at high (6 LPM) and low (2 LPM) flow rates. The initial flow rate was randomly assigned as either high or low, and then alternated between the two. A clinically significant change in CO2 level was defined as a 5-mmHg difference.
Results: A total of 48 ΔtcCO2 measurements were recorded following changes in HFNV flow rate in preterm infants (mean±SD: 28.1±2.6 weeks’ gestation, 1050±328 g at birth). The mean ΔtcCO2 (95% confidence interval) was -1.1 mmHg (-2.3 to 0.1) when increasing flow from low to high and 0.46 mmHg (-0.49 to 1.41) when decreasing flow from high to low, as measured 3 hours after the change. Using an equivalence trial approach, the 95% confidence interval excluded a difference greater than 5 mmHg, indicating no clinically significant difference in tcCO2 readings (see figure). No significant changes were observed in spontaneous respiratory rate, FiO2, desaturation, apnea, or bradycardia events; however, mean oxygen saturation increased with 6 LPM (p < 0.05).
Conclusion(s): In stable preterm infants supported by HFNV, altering the flow rate by a factor of three (either increasing or decreasing) did not significantly impact tcCO2 levels within 3 hours post-change. These findings may influence ventilation management in premature infants with hypercarbia or hypocarbia, but require further validation in studies involving unstable preterm infants and a larger cohort.
Equivalence trial results - Possible scenarios and results of this study
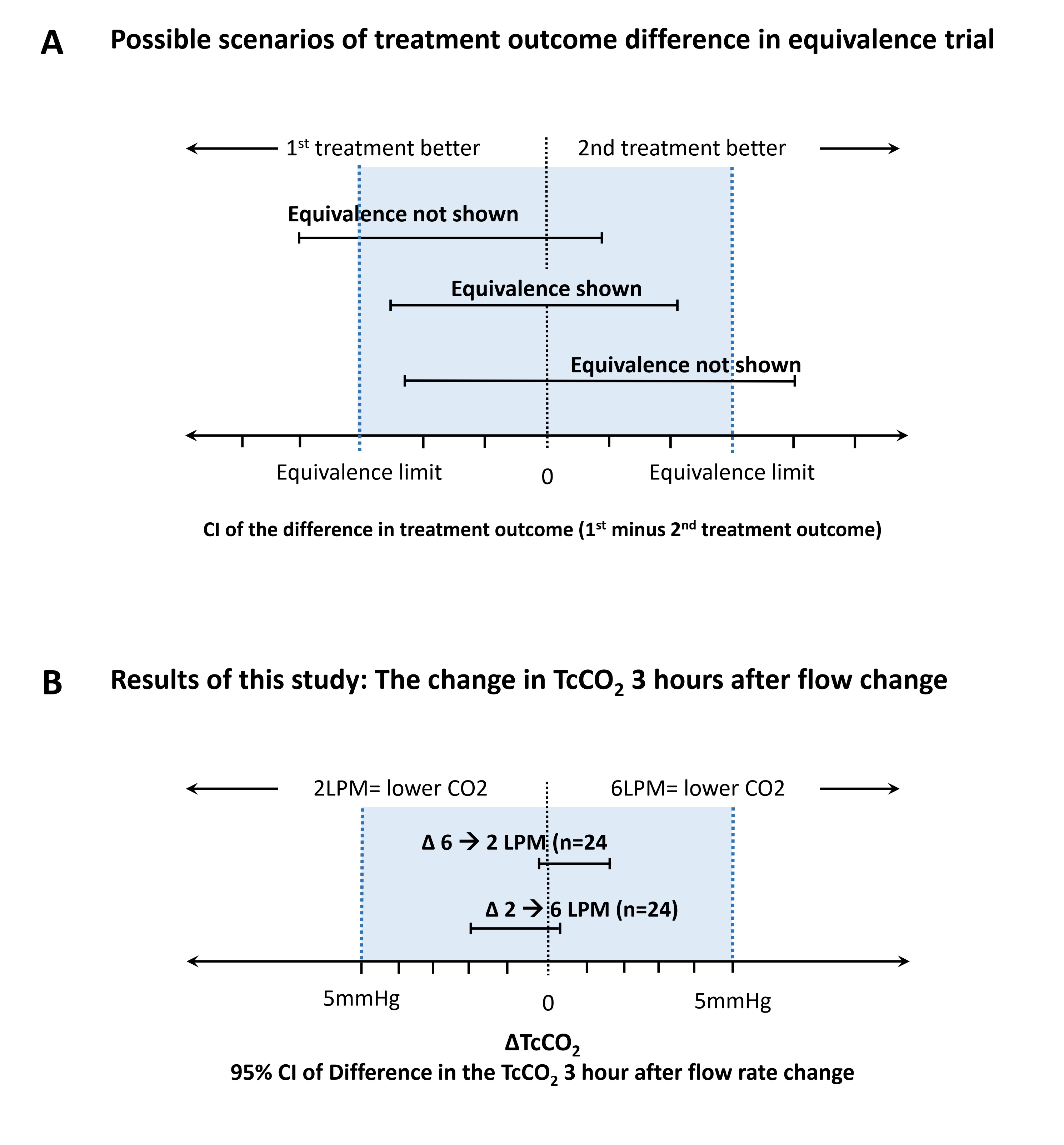 A. Possible scenarios of results for a Equivalence trial according to Piaggio et al. (2012, JAMA)
A. Possible scenarios of results for a Equivalence trial according to Piaggio et al. (2012, JAMA)B. Results of this study: the change in TcCO2 3 hours after flow rate change
Error bars = 95% confidence interval of Difference in the TcCO2 3 hours after flow rate change
TcCO2; transcutaneous CO2, LPM; Liter per minute, CI; confidence interval
Equivalence trial results - Possible scenarios and results of this study
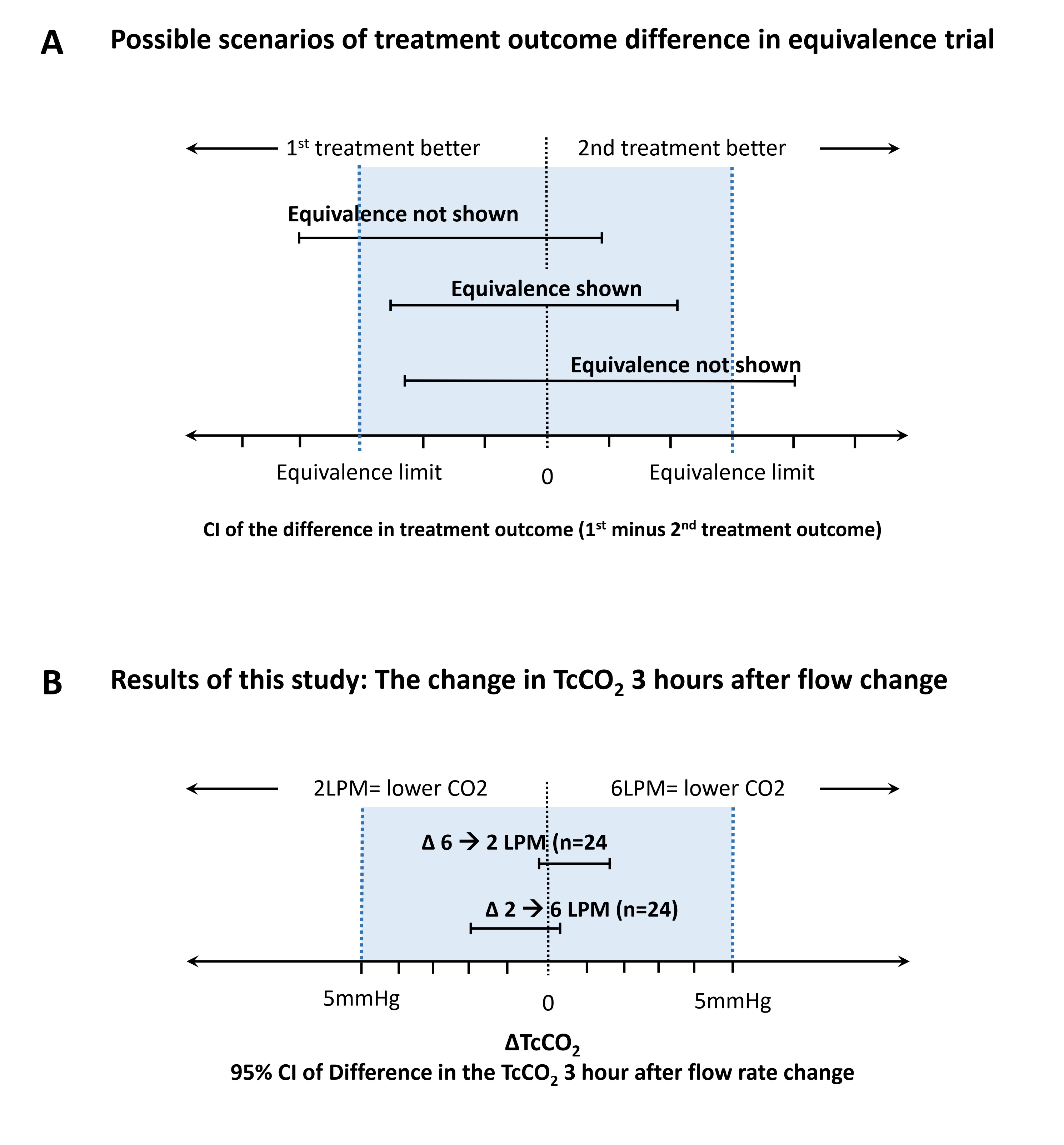 A. Possible scenarios of results for a Equivalence trial according to Piaggio et al. (2012, JAMA)
A. Possible scenarios of results for a Equivalence trial according to Piaggio et al. (2012, JAMA)B. Results of this study: the change in TcCO2 3 hours after flow rate change
Error bars = 95% confidence interval of Difference in the TcCO2 3 hours after flow rate change
TcCO2; transcutaneous CO2, LPM; Liter per minute, CI; confidence interval

