Neonatal Neurology 3
Session: Neonatal Neurology 3
366 - Clinical and histologic chorioamnionitis are associated with an increased risk of encephalopathy among neonates with metabolic acidosis at birth: A cohort study.
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 366.4117
Marie Cornet, UCSF Benioff Children's Hospital San Francisco, San Francisco, CA, United States; MICHAEL W. KUZNIEWICZ, Kaiser Permanante, Los Gatos, CA, United States; Aditi Lahiri, Kaiser Permanente, Division of Research, Berkeley, CA, United States; Stephanie L. Gaw, University of California, San Francisco, San Francisco, CA, United States; Yvonne W. Wu, UCSF, San Francisco, CA, United States
- MC
Marie Cornet, MD, PhD (she/her/hers)
Assistant Professor
University of California, San Francisco, School of Medicine
San Francisco, California, United States
Presenting Author(s)
Background: Therapeutic hypothermia (TH) is the standard of care in neonates with acidosis and moderate to severe neonatal encephalopathy (NE). To ensure infants eligible for TH are identified, many hospitals have instituted standardized neurologic assessments in neonates with acidosis. Chorioamnionitis is a risk factor for hypoxic-ischemic encephalopathy, but it is unclear if this is due to increased acidosis risk or an alternative pathway.
Objective: To evaluate whether chorioamnionitis exposure increases NE risk after adjusting for acidosis severity.
Design/Methods: Population-based cohort study of neonates > 35 weeks with perinatal acidosis (cord pH < 7 or base deficit >10 on any gas within 2 hours after birth) born at one of 15 Kaiser Permanente Northern California hospitals (01/2012-07/2019). Acidosis severity was defined by the worst base deficit on any cord of infant gas within 2 hours after birth. Clinical chorioamnionitis (CC) was defined by ICD codes, and histologic chorioamnionitis (HC) was identified from placenta pathology reports. NE was defined as having an abnormal standardized neurologic examination after birth. We used Poisson regression with robust standard error clustered by hospital to assess the association between CC or HC, and NE and other secondary neonatal outcomes, adjusting for clinical characteristics and acidosis severity.
Results: Among 4,227 infants with neonatal acidosis (population incidence 1.5%), 1,086 (26%) were exposed to CC. Characteristics of neonates exposed and unexposed to CC are described in Table 1. Placenta pathology was available for 2,064 (49%), with HC found in 1,129 (55%). NE occurred in 702 infants (17%), including 359 (8.5%) treated with TH. NE prevalence increased with acidosis severity (Figure 1). CC exposure was associated with higher NE rates, even after adjusting for the degree of acidosis and potential confounders (Figure 1A – Table 2). Among neonates with placenta pathology, HC was associated with increased NE and TH risks, even after adjusting for the acidosis severity and confounders (Figure 1B – Table 2). Of note, among 1,132 neonates unexposed to CC with placenta available, those exposed to HC still had a higher risk of NE (RR 1.45 - 95% CI 1.22-1.72) that persisted after adjusting for clinical characteristics and acidosis severity (aRR 1.47 -95% CI 1.20-1.80).
Conclusion(s): In this large cohort, nearly a fifth of neonates with acidosis had NE. Chorioamnionitis, both clinical and histologic, appeared to increase the risk of NE beyond acidosis severity, suggesting it may amplify the effect of a similar initial injury.
Table 1: Comparison of infants exposed and unexposed to clinical chorioamnionitis among 4,227 infants born with acidosis
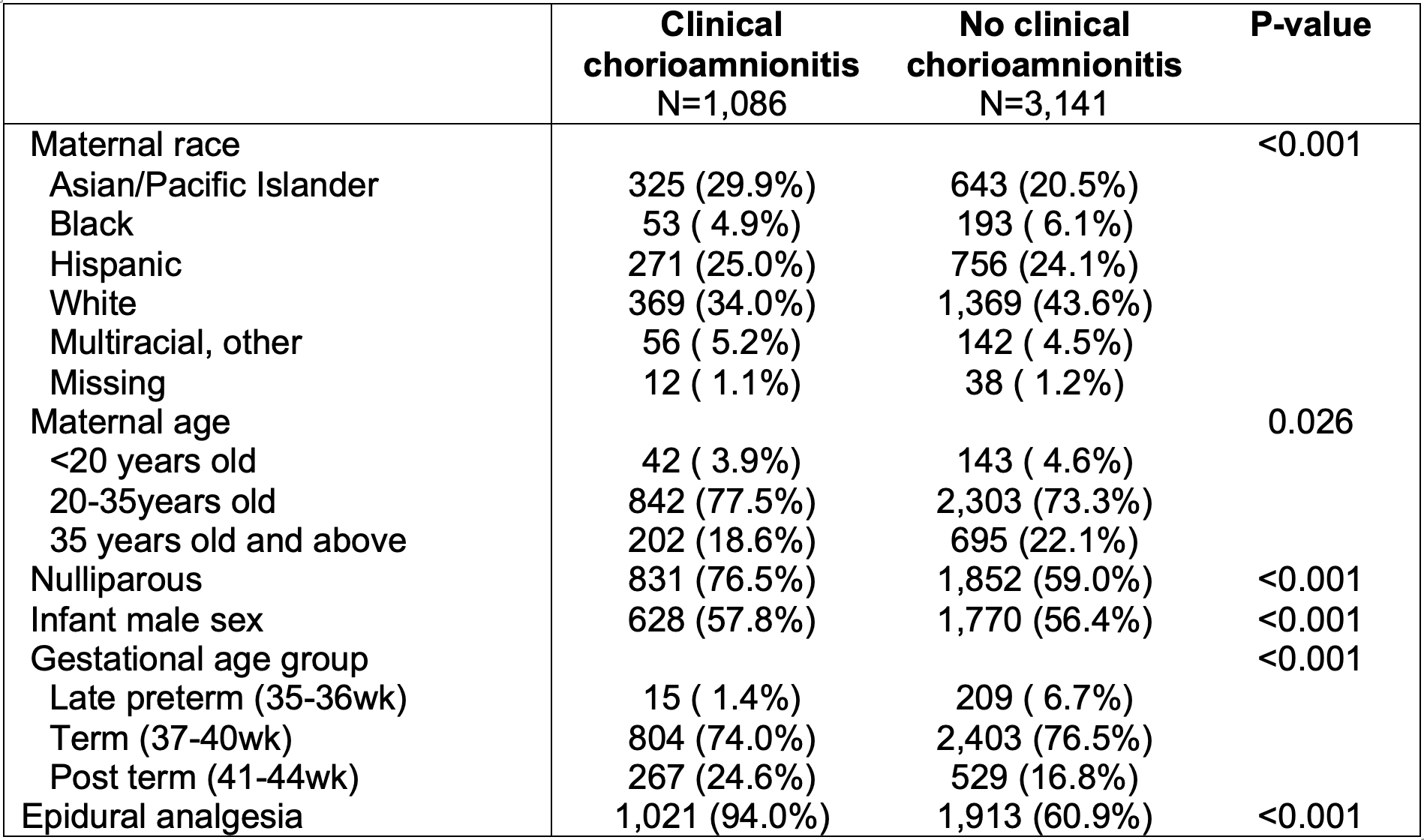
Table 2: RR and adjusted odds ratio of adverse neonatal outcomes between neonates with and without exposure to clinical and histologic chorioamnionitis.
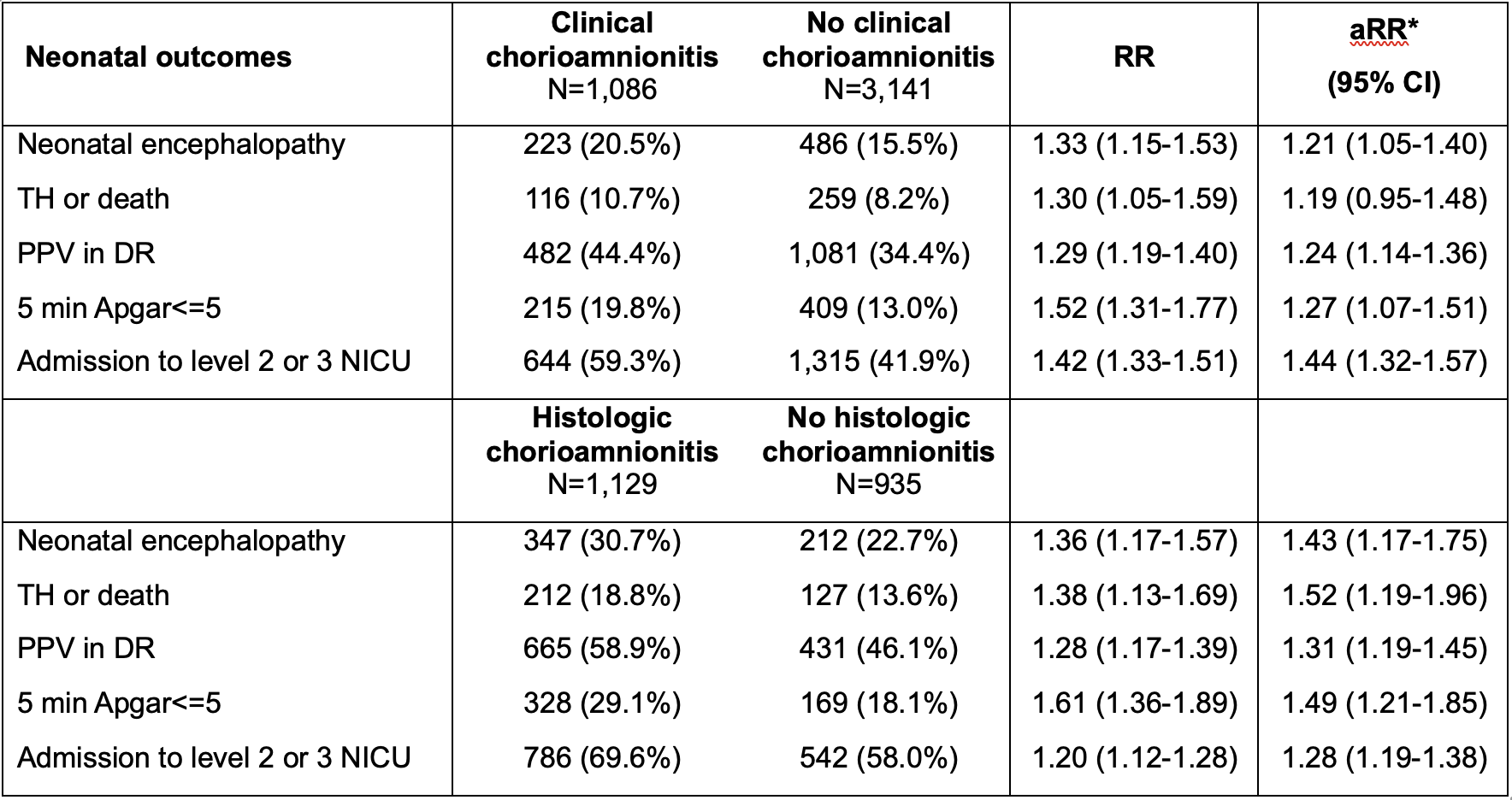 * aRR (adjusted relative risk) calculated by Poisson regression with robust standard error clustered by the hospital and adjusting for all factors included in Table 1: race, maternal age, parity status, infant sex, gestational age, epidural, and degree of acidosis as a spline.
* aRR (adjusted relative risk) calculated by Poisson regression with robust standard error clustered by the hospital and adjusting for all factors included in Table 1: race, maternal age, parity status, infant sex, gestational age, epidural, and degree of acidosis as a spline. Figure 1: Probability of encephalopathy based on degree of acidosis stratified by clinical chorioamnionitis(A) and histologic chorioamnionitis.
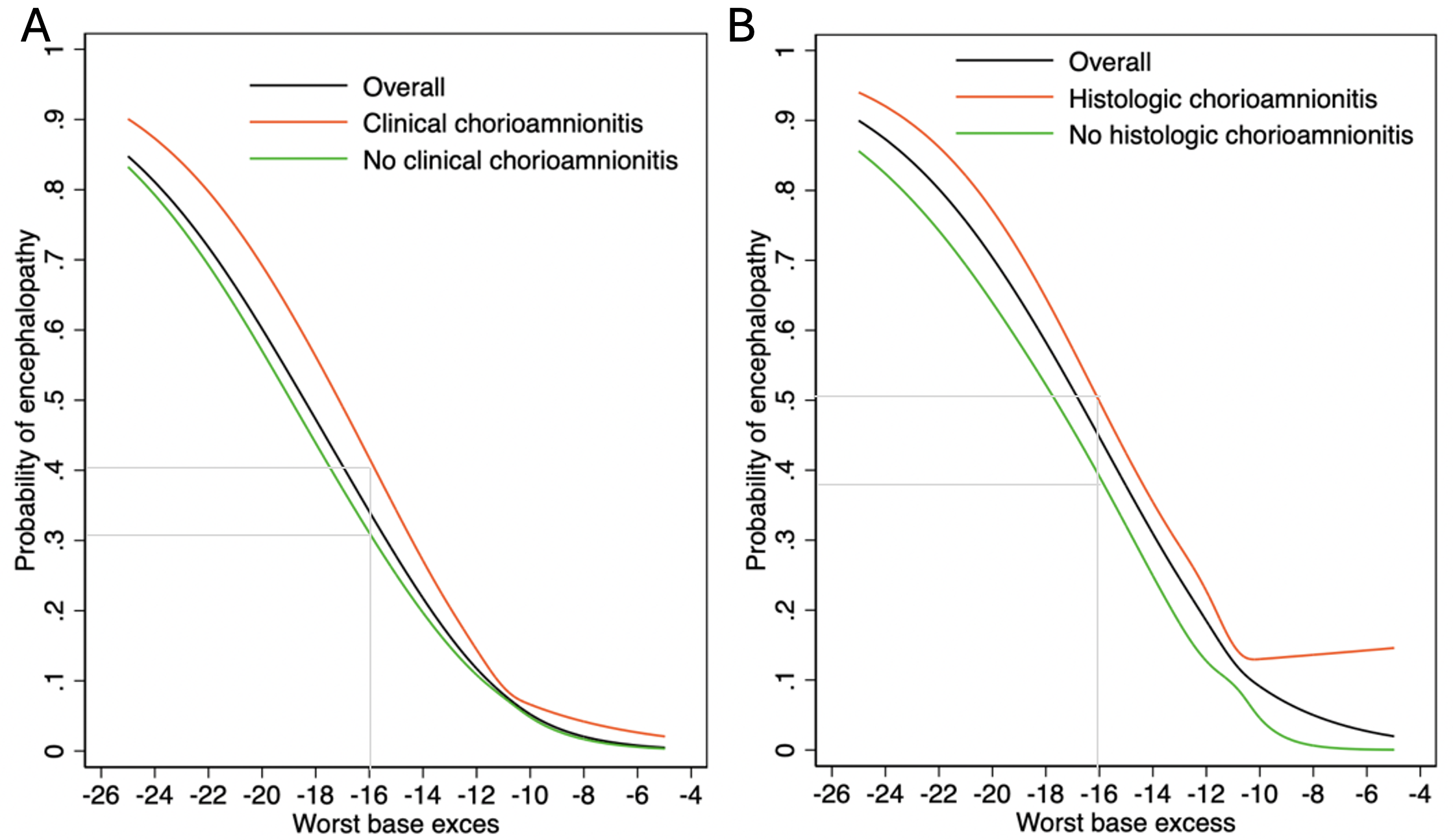 The probability was calculated by constructing a logistic regression model, adjusting for the worst base excess (BE) as a spline. For a worst BE of -16, 42% of infants exposed to clinical chorioamnionitis had encephalopathy compared to 31% of unexposed infants (Risk difference 8.4% [95%CI 4.2-12.6%]). Similarly, among infants with a placenta available, for a worst BE of -16, 51% of infants exposed to histologic chorioamnionitis had encephalopathy compared to 38% of unexposed infants (Risk difference 15.1% [95%CI 9.8-20.4%]).
The probability was calculated by constructing a logistic regression model, adjusting for the worst base excess (BE) as a spline. For a worst BE of -16, 42% of infants exposed to clinical chorioamnionitis had encephalopathy compared to 31% of unexposed infants (Risk difference 8.4% [95%CI 4.2-12.6%]). Similarly, among infants with a placenta available, for a worst BE of -16, 51% of infants exposed to histologic chorioamnionitis had encephalopathy compared to 38% of unexposed infants (Risk difference 15.1% [95%CI 9.8-20.4%]). Table 1: Comparison of infants exposed and unexposed to clinical chorioamnionitis among 4,227 infants born with acidosis
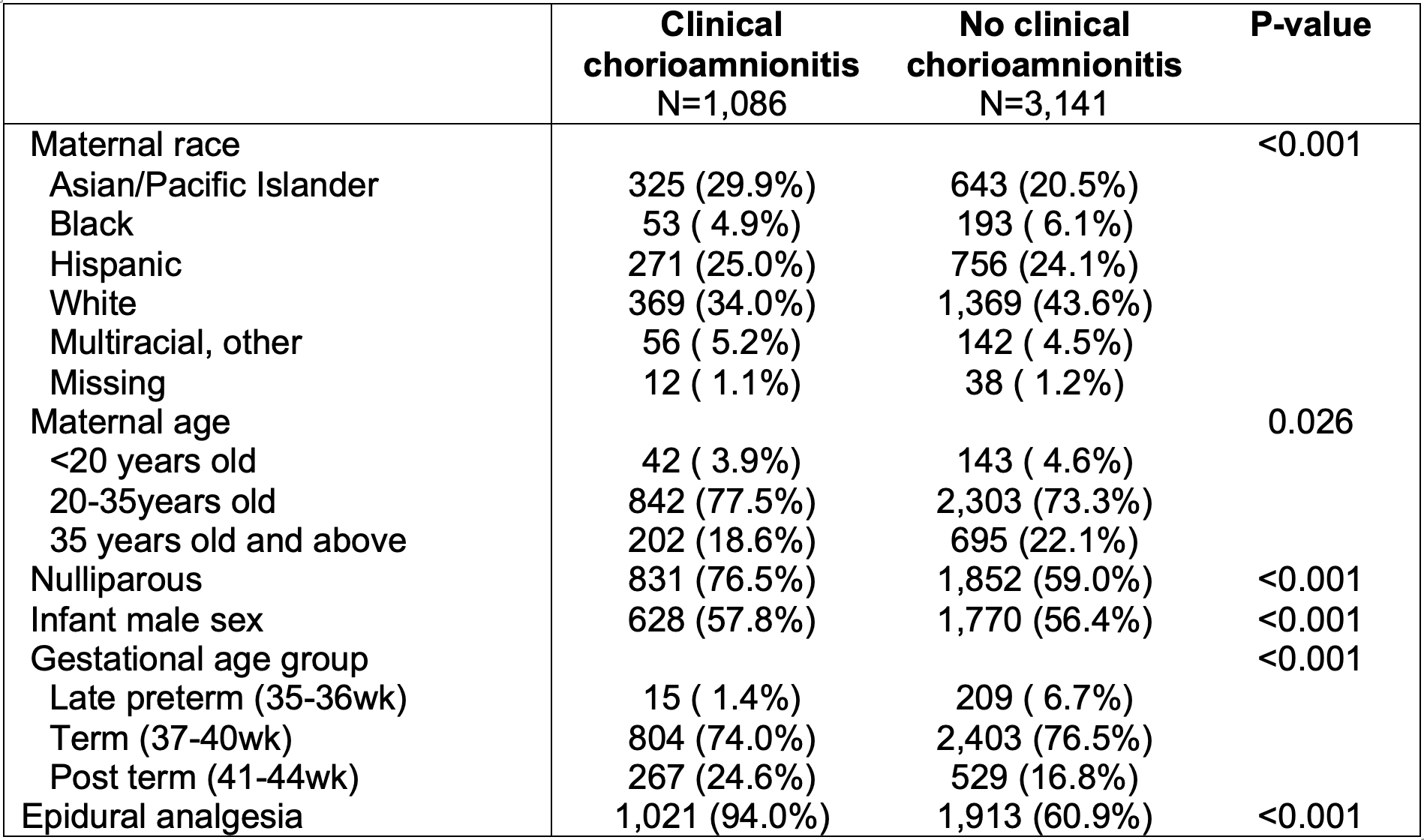
Table 2: RR and adjusted odds ratio of adverse neonatal outcomes between neonates with and without exposure to clinical and histologic chorioamnionitis.
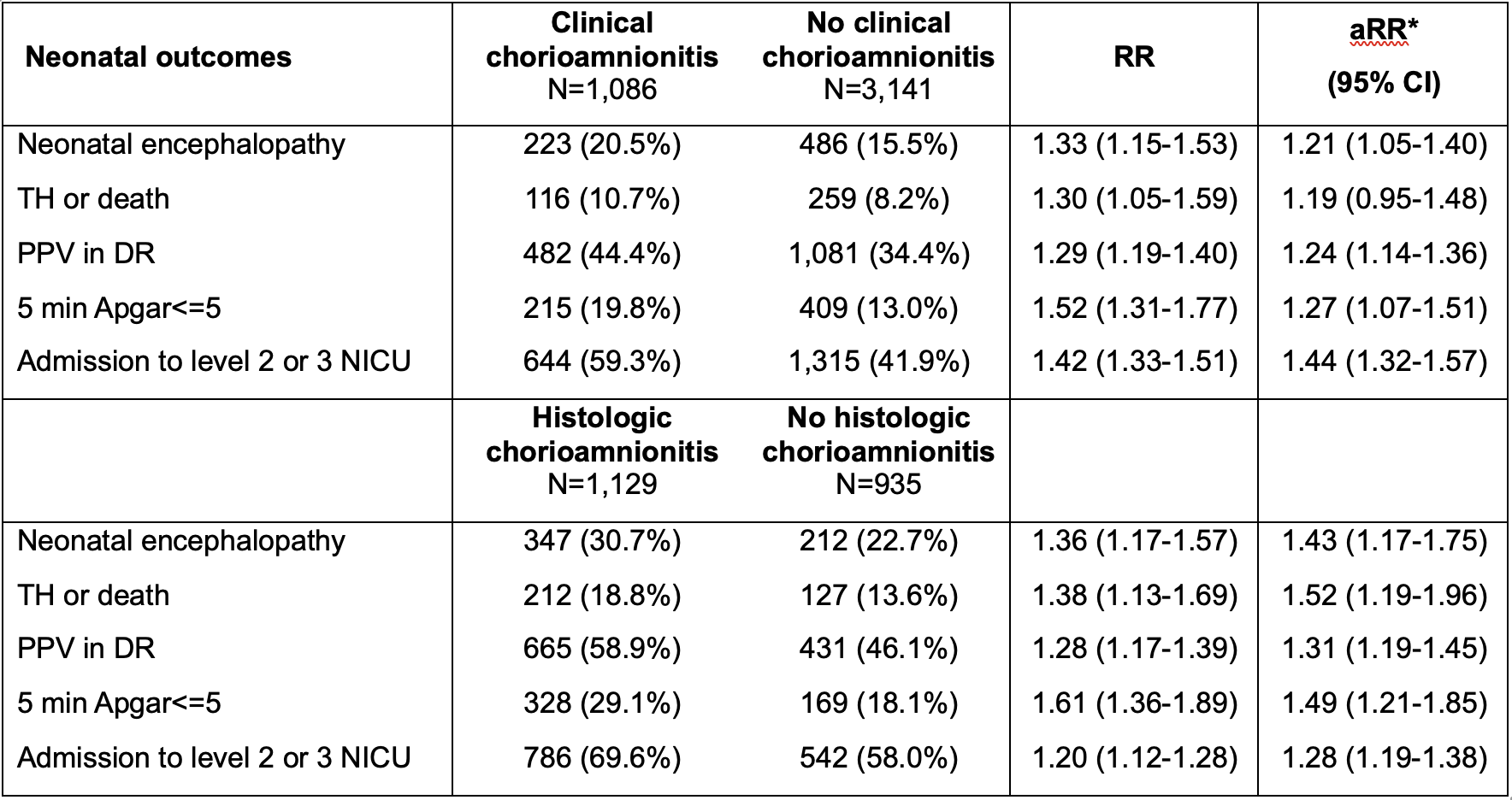 * aRR (adjusted relative risk) calculated by Poisson regression with robust standard error clustered by the hospital and adjusting for all factors included in Table 1: race, maternal age, parity status, infant sex, gestational age, epidural, and degree of acidosis as a spline.
* aRR (adjusted relative risk) calculated by Poisson regression with robust standard error clustered by the hospital and adjusting for all factors included in Table 1: race, maternal age, parity status, infant sex, gestational age, epidural, and degree of acidosis as a spline. Figure 1: Probability of encephalopathy based on degree of acidosis stratified by clinical chorioamnionitis(A) and histologic chorioamnionitis.
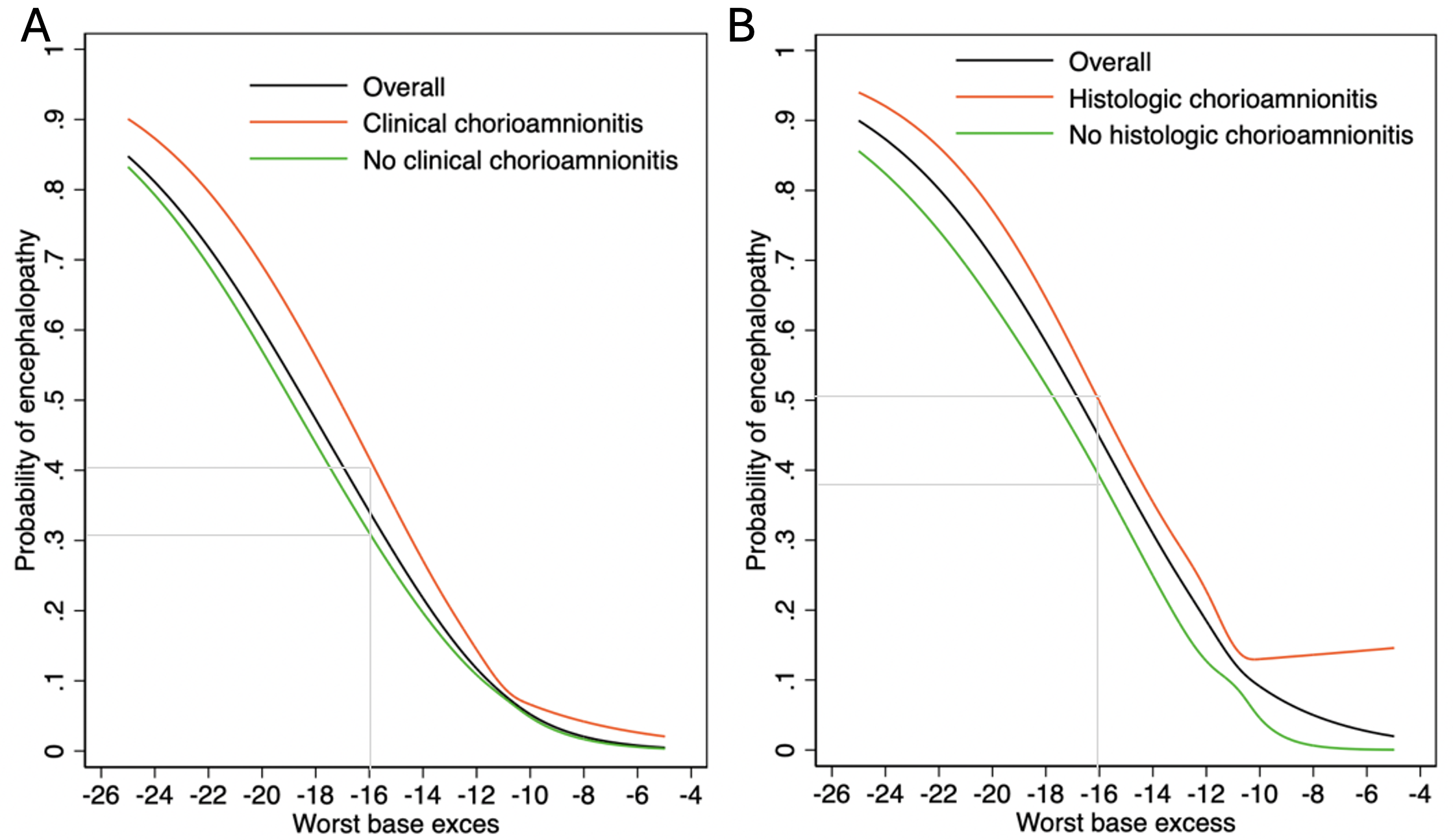 The probability was calculated by constructing a logistic regression model, adjusting for the worst base excess (BE) as a spline. For a worst BE of -16, 42% of infants exposed to clinical chorioamnionitis had encephalopathy compared to 31% of unexposed infants (Risk difference 8.4% [95%CI 4.2-12.6%]). Similarly, among infants with a placenta available, for a worst BE of -16, 51% of infants exposed to histologic chorioamnionitis had encephalopathy compared to 38% of unexposed infants (Risk difference 15.1% [95%CI 9.8-20.4%]).
The probability was calculated by constructing a logistic regression model, adjusting for the worst base excess (BE) as a spline. For a worst BE of -16, 42% of infants exposed to clinical chorioamnionitis had encephalopathy compared to 31% of unexposed infants (Risk difference 8.4% [95%CI 4.2-12.6%]). Similarly, among infants with a placenta available, for a worst BE of -16, 51% of infants exposed to histologic chorioamnionitis had encephalopathy compared to 38% of unexposed infants (Risk difference 15.1% [95%CI 9.8-20.4%]). 
