Neonatal Hemodynamics and Cardiovascular Medicine 2
Session: Neonatal Hemodynamics and Cardiovascular Medicine 2
050 - Effect of Temperature on Pulmonary Vascular Resistance in an Ovine Model of Persistent Pulmonary Hypertension of the Newborn (PPHN)
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 50.5024
Rebecca Valdez, University of California Davis, Davis, CA, United States; Munmun Rawat, University at Buffalo, Buffalo, NY, United States; Praveen Chandrasekharan, Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo, Buffalo, NY, United States; Evan M. Giusto, UC Davis Health, Sacramento, CA, United States; Amy Lesneski, University of California, Davis, School of Medicine, Davis, CA, United States; Victoria Hammitt, University of California, Davis, School of Medicine, Sacramento, CA, United States; Erin Riley, University of California, Davis, School of Medicine, Redding, CA, United States; Morgan Hardie, University of California, Davis, School of Medicine, Davis, CA, United States; Paulina Hume, University of California Davis Children's Hospital, 612 El Dorado Way, CA, United States; Sylvia Bowditch, University of California Davis Children's Hospital, Sacramento, CA, United States; Payam Vali, University of California, Davis, School of Medicine, sacramento, CA, United States; Satyan Lakshminrusimha, UC Davis, Sacramento, CA, United States; Deepika Sankaran, University of California Davis Children's Hospital, Sacramento, CA, United States

Rebecca Valdez, B.S. (she/her/hers)
Trainee
University of California Davis
Davis, California, United States
Presenting Author(s)
Background: Therapeutic hypothermia of 33.5˚C is the standard of care in the management of hypoxic ischemic encephalopathy (HIE). Persistent pulmonary hypertension of the newborn (PPHN), often secondary to meconium aspiration syndrome (MAS), is observed in 20–25% of term infants with moderate to severe HIE. Hypothermia may increase the pulmonary vascular resistance (PVR) and potentially worsen PPHN.
Objective: To determine the effect of hypothermia (33.5˚C) and normothermia (36.5-37.5˚C) on pulmonary vascular resistance in an ovine model of PPHN induced by MAS.
Design/Methods: Asphyxia was induced by meconium instillation and umbilical cord occlusion to induce MAS and PPHN in 20 fetal lambs (134-141 days gestational age). Lambs were resuscitated per neonatal resuscitation program guidelines. Thirteen lambs were maintained normothermic (36.5-37.5˚C), while hypothermia (33.5˚C) was induced using a cooling blanket in 7 lambs for 6 hours and inspired oxygen was titrated to achieve target preductal oxygen saturation of 90-98%. Hemodynamics including left carotid artery blood flow (CaF), mean blood pressure (BP), left pulmonary artery blood flow and main pulmonary artery pressure were monitored, and PVR was calculated
Results: The baseline characteristics were not different between the normothermic and hypothermic lambs (Table). Goal temperature of 33.5˚ C was achieved by 2 hours after birth in hypothermic lambs and remained lower between 2-6 hours than normothermic lambs (p < 0.001). Hypothermic lambs had significantly higher PVR than normothermic lambs between 2-6 hours after birth (p= 0.008, Figure 1). The mean BP and CaF were higher in normothermic lambs between 2-6 hours after birth (p < 0.05, Figure 2 and 3).
Conclusion(s): Hypothermia is associated with higher PVR in neonatal lambs with MAS, PPHN and HIE. Close hemodynamic monitoring is warranted in neonates with MAS, PPHN and HIE managed with therapeutic hypothermia. Randomized trials are needed to study the effect of hypothermia on cardiorespiratory outcomes.
Baseline characteristics between normothermic and hypothermic lambs with MAS, HIE and PPHN
.jpg)
Comparison of temperature between normothermic and hypothermic lambs between 0.5 to 6 hours after birth.
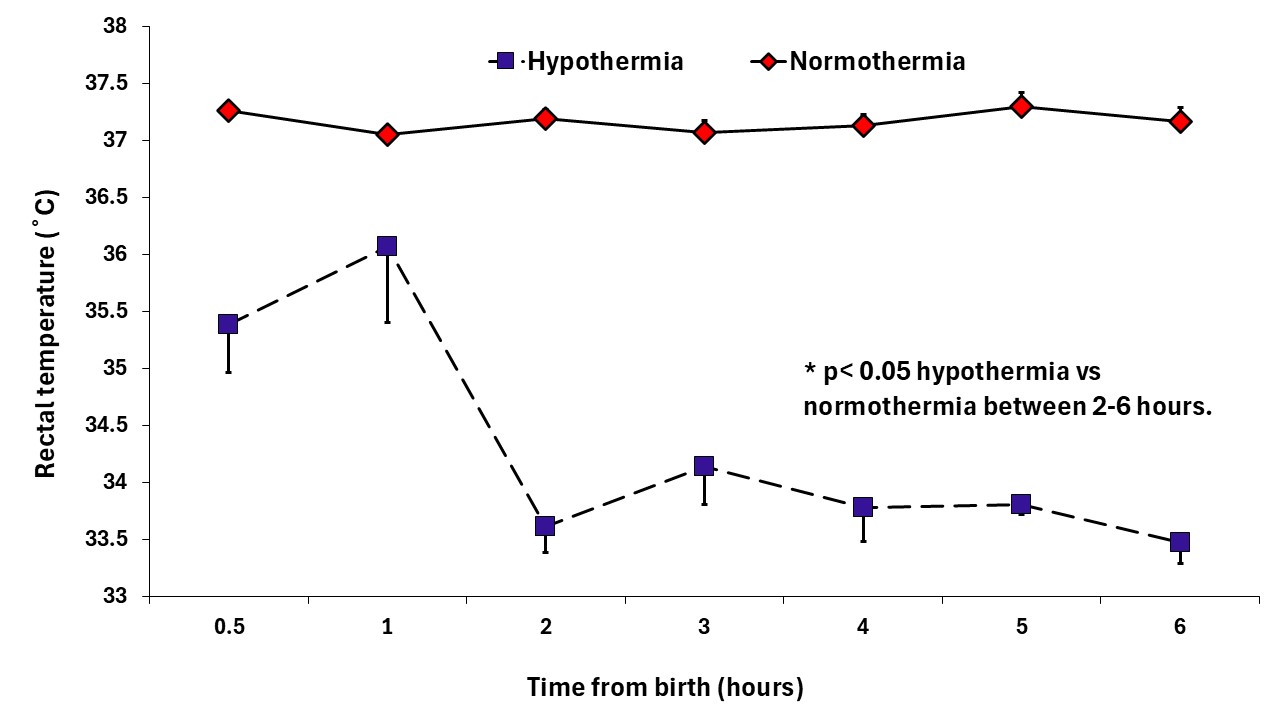 Temperature was significantly lower in hypothermic lambs between 2-6 hours after birth compared to normothermic lambs (p < 0.001).
Temperature was significantly lower in hypothermic lambs between 2-6 hours after birth compared to normothermic lambs (p < 0.001).Comparison of pulmonary vascular resistance (PVR, figure 2a), left carotid artery blood flow (figure 2b) and mean blood pressure (figure 2c) between normothermic and hypothermic lambs between 0.5 to 6 hours after birth.
.jpg) Higher PVR (figure 2a, p= 0.008), lower left carotid artery blood flow (figure 2b, p= 0.0005) and lower mean blood pressure (figure 2c, p= 0.046) were observed in hypothermic lambs between 2-6 hours after birth compared to normothermic lambs.
Higher PVR (figure 2a, p= 0.008), lower left carotid artery blood flow (figure 2b, p= 0.0005) and lower mean blood pressure (figure 2c, p= 0.046) were observed in hypothermic lambs between 2-6 hours after birth compared to normothermic lambs.
